The human body’s intricate network of nerves relies heavily on four major nerve plexuses that distribute signals across various regions, ensuring coordinated movement and sensation. These nerve plexuses, including the cervical, brachial, lumbar, and sacral complexes, originate from the spinal cord and extend to the head, arms, and legs, playing a vital role in both voluntary and involuntary functions. This article delves into their anatomical structure and physiological significance, offering a detailed guide to understanding their contributions to the peripheral nervous system.
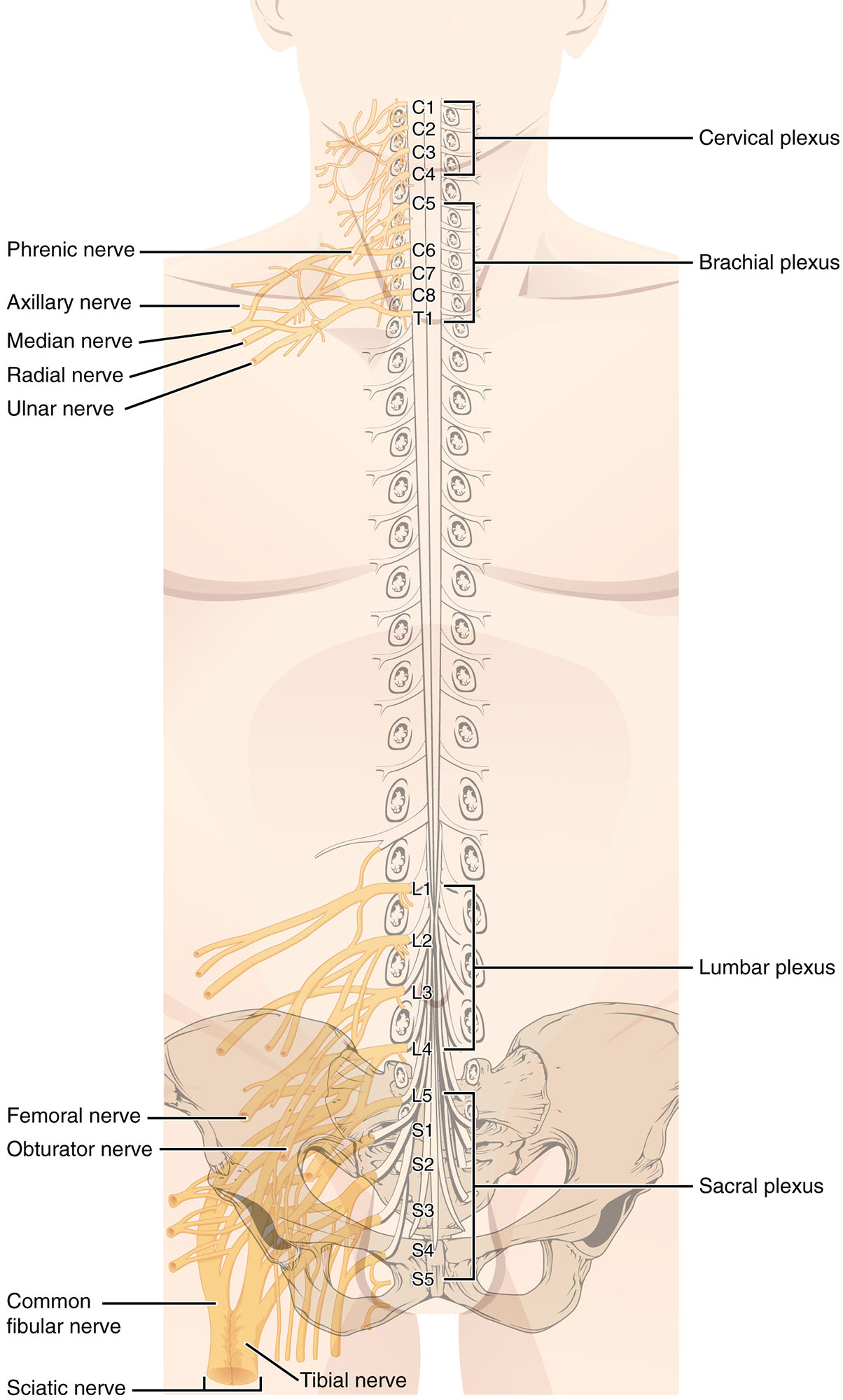
Labeled Parts of the Nerve Plexuses
Cervical plexus The cervical plexus arises from the upper spinal nerves (C1-C4) and provides innervation to the posterior head, neck, and diaphragm. It is crucial for movements such as neck rotation and for the phrenic nerve’s role in respiratory function by controlling the diaphragm.
Brachial plexus The brachial plexus, formed by spinal nerves C5-T1, supplies the upper limb, including the shoulder, arm, and hand. It gives rise to major nerves like the median and ulnar, which are essential for fine motor skills and sensory feedback from the hand.
Phrenic nerve The phrenic nerve originates from the cervical plexus (C3-C5) and is the primary nerve for diaphragmatic movement, critical for breathing. Damage to this nerve can lead to respiratory difficulties, highlighting its indispensable role in pulmonary function.
Axillary nerve The axillary nerve, a branch of the brachial plexus, innervates the deltoid muscle and teres minor, facilitating shoulder abduction and external rotation. It also provides sensory input to the skin over the deltoid region, aiding in proprioception.
Median nerve The median nerve, derived from the brachial plexus, supplies the flexor muscles of the forearm and most of the hand’s intrinsic muscles, enabling gripping and precision movements. It carries sensory information from the thumb, index, and middle fingers, making it vital for dexterity.
Radial nerve The radial nerve, another brachial plexus branch, innervates the extensor muscles of the arm and hand, allowing for extension at the elbow, wrist, and fingers. It also provides sensory innervation to the posterior arm and hand, supporting motor control and sensation.
Ulnar nerve The ulnar nerve, originating from the brachial plexus, supplies the intrinsic hand muscles and flexor carpi ulnaris, crucial for finger abduction and adduction. It also provides sensation to the ring and pinky fingers, and its compression can cause the characteristic “funny bone” sensation.
Lumbar plexus The lumbar plexus, formed by spinal nerves L1-L4, innervates the anterior thigh and parts of the lower abdomen, supporting hip flexion and knee extension. It gives rise to nerves like the femoral and obturator, which are essential for leg movement.
Femoral nerve The femoral nerve, a branch of the lumbar plexus, innervates the quadriceps femoris and other anterior thigh muscles, enabling knee extension and hip flexion. It also provides sensory input to the anterior thigh and medial leg, contributing to gait stability.
Obturator nerve The obturator nerve, arising from the lumbar plexus, supplies the adductor muscles of the thigh, facilitating leg adduction and stabilization. It also carries sensory fibers to the medial thigh, supporting proprioceptive feedback during movement.
Sacral plexus The sacral plexus, derived from spinal nerves L4-S4, innervates the posterior leg and pelvic region, including the gluteal muscles and hamstrings. It is the origin of the sciatic nerve, which plays a key role in lower limb mobility.
Common fibular nerve The common fibular nerve, a branch of the sciatic nerve from the sacral plexus, innervates the anterior and lateral leg muscles, enabling foot dorsiflexion and eversion. It provides sensory innervation to the lateral leg and dorsum of the foot, critical for balance.
Tibial nerve The tibial nerve, also from the sciatic nerve via the sacral plexus, supplies the posterior leg and foot muscles, facilitating plantar flexion and inversion. It carries sensory fibers to the sole of the foot, supporting tactile sensation during walking.
Sciatic nerve The sciatic nerve, the largest nerve in the body and a major branch of the sacral plexus, innervates the posterior thigh, leg, and foot via its tibial and common fibular branches. It is vital for lower limb movement and can be a site of compression leading to sciatica.
Anatomical Overview of Nerve Plexuses
The nerve plexuses form complex networks that interconnect spinal nerve roots, enhancing the distribution of motor and sensory signals. This intricate arrangement ensures efficient communication between the central nervous system and peripheral regions.
- Spinal cord origins: Each plexus arises from specific spinal segments, with the cervical plexus starting at C1-C4 and the sacral plexus extending to S4, reflecting their regional specialization.
- Interweaving structure: The plexuses consist of ventral rami that merge and split, creating a web-like pattern that distributes nerves to multiple muscles and skin areas.
- Functional zones: The upper plexuses (cervical and brachial) serve the head, neck, and arms, while the lower plexuses (lumbar and sacral) target the pelvis and legs, aligning with anatomical divisions.
- Protective pathways: Nerves travel through fascial planes and bony structures, such as the brachial plexus passing under the clavicle, offering some protection but also vulnerability to injury.
Physiological Roles and Functions
Nerve plexuses are integral to both voluntary movement and involuntary reflexes, coordinating a wide array of bodily functions. Their mixed composition of motor, sensory, and autonomic fibers allows for versatile control.
- Motor control: The brachial plexus drives arm movements via nerves like the radial and median, while the sacral plexus supports leg motion through the sciatic nerve.
- Sensory feedback: Sensory nerves, such as the ulnar and femoral, transmit touch, pain, and temperature sensations to the spinal cord for processing.
- Autonomic regulation: The phrenic nerve, part of the cervical plexus, regulates diaphragmatic breathing, an essential autonomic function.
- Reflex arcs: Plexuses facilitate rapid responses, such as the knee-jerk reflex involving the femoral nerve, enhancing stability and safety.
- Muscle coordination: Multiple nerve branches from each plexus ensure synchronized muscle action, such as the axillary nerve’s role in shoulder stability.
Clinical Significance and Examination
Assessing nerve plexus function is a key aspect of neurological evaluations, helping to identify damage or dysfunction. These assessments often involve testing strength, sensation, and reflexes associated with specific nerves.
- Injury sites: The brachial plexus can be injured during shoulder trauma, leading to Erb’s palsy, while sciatic nerve compression causes sciatica.
- Diagnostic techniques: Electromyography (EMG) and nerve conduction studies evaluate plexus integrity, pinpointing lesions or entrapments.
- Symptom recognition: Numbness in the hand may indicate median nerve issues, while foot drop suggests common fibular nerve impairment.
- Therapeutic approaches: Physical therapy and surgical decompression can address plexus injuries, depending on the extent and location.
Developmental and Evolutionary Insights
The development of nerve plexuses reflects the evolutionary adaptation of the nervous system to support upright posture and complex limb movements. Their formation during embryogenesis involves precise neural crest migration and differentiation.
- Embryonic origins: Plexuses form as ventral rami reorganize, with the lumbar and sacral plexuses adapting to bipedal locomotion in humans.
- Species variation: In quadrupeds, the brachial and sacral plexuses are more balanced, while humans emphasize the sacral plexus for leg dominance.
- Congenital anomalies: Conditions like Klumpke’s palsy, affecting the lower brachial plexus, can arise from birth injuries, underscoring developmental vulnerabilities.
In conclusion, the nerve plexuses of the body represent a remarkable integration of anatomy and physiology, enabling the seamless operation of limbs and vital organs. Their detailed structure, as illustrated in this anatomical image, provides a foundation for understanding both normal function and potential pathologies, making them a critical focus for ongoing study and clinical practice.

