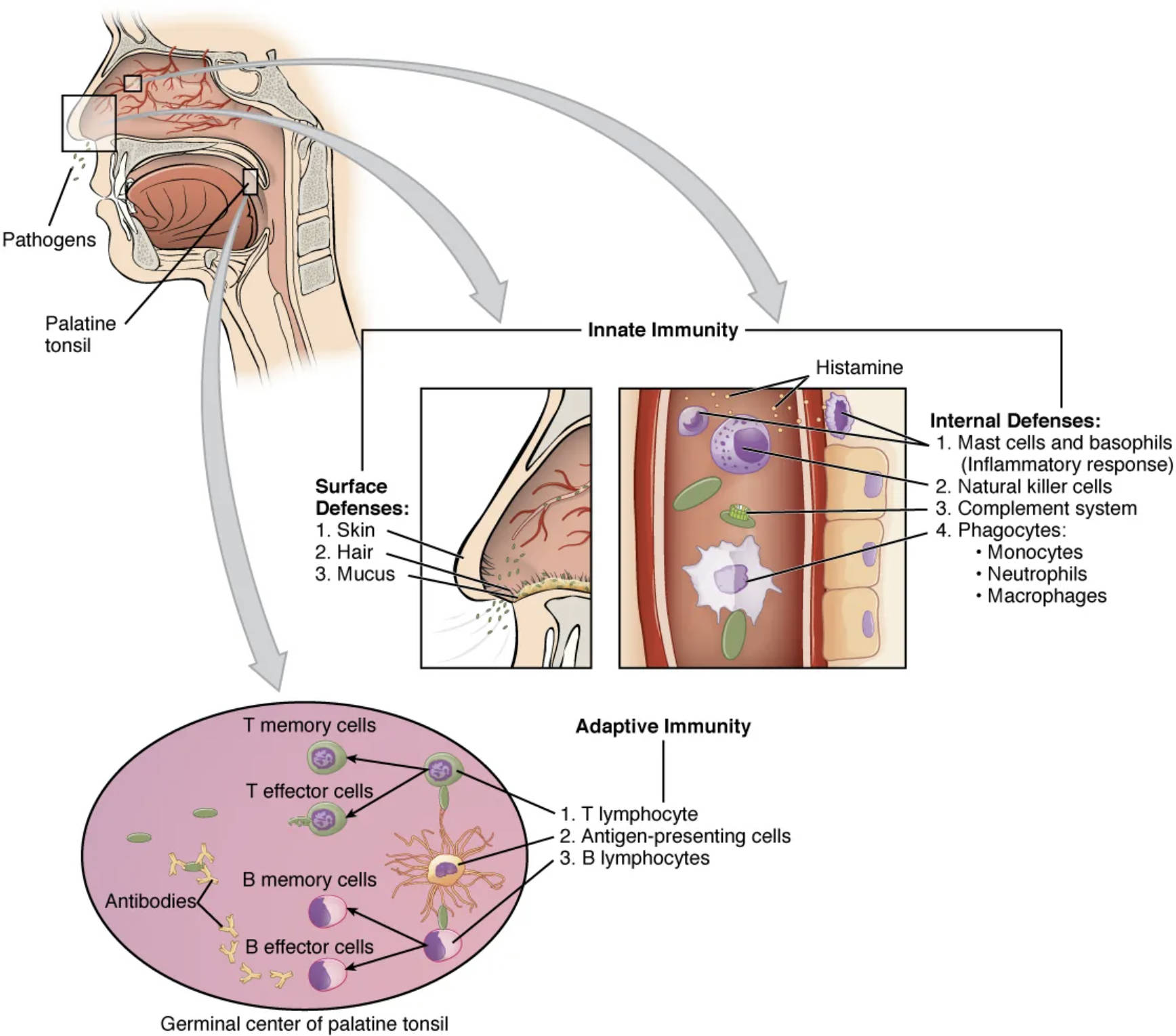
The immune system relies on a dynamic partnership between innate and adaptive immunity to protect the body from pathogens, with the tonsils playing a pivotal role as the first line of defense. Located in the throat, the palatine tonsil and its germinal center are key sites where these two immune branches collaborate, trapping pathogens and initiating both immediate and long-term responses. This illustration highlights the intricate interplay of cellular and molecular mechanisms that ensure robust protection against infections.
Labeled Components of the Immune Response
Palatine tonsil: Positioned on either side of the throat, this lymphoid tissue traps pathogens entering through the mouth or nose. It serves as a critical site for initiating both innate and adaptive immune responses.
Pathogens: These disease-causing microorganisms, such as bacteria and viruses, enter the body via the respiratory or digestive tracts. They trigger the activation of immune defenses, prompting a coordinated response.
Surface Defenses: Comprising skin, hair, and mucus, these physical barriers prevent pathogen entry into the body. They act as the first layer of innate immunity, reducing the initial microbial load.
Skin: The outermost layer of the body, skin provides a physical barrier against pathogens. It also secretes antimicrobial substances, enhancing innate protection.
Hair: Found in the nasal passages, hair traps airborne pathogens, preventing them from reaching deeper tissues. This mechanical defense supports the mucosal immune response.
Mucus: Produced in the respiratory and digestive tracts, mucus traps pathogens and facilitates their removal via cilia. It works synergistically with other surface defenses to limit infection.
Innate Immunity: This rapid, non-specific immune response involves cells like mast cells and phagocytes. It provides immediate protection while activating adaptive immunity.
Histamine: Released by mast cells and basophils, histamine triggers inflammation to recruit immune cells to the infection site. It plays a key role in the early innate response.
Internal Defenses: These include mast cells, natural killer cells, the complement system, and phagocytes. They work together to neutralize pathogens within the body.
Mast cells and basophils: These cells release histamine and other chemicals to initiate inflammation. They are essential for alerting the immune system to pathogen presence.
Natural killer cells: These lymphocytes target and destroy infected or cancerous cells. They provide a rapid innate defense against viral infections.
Complement system: A group of proteins that enhance immune responses by marking pathogens for destruction. It amplifies the effects of phagocytes and natural killer cells.
Phagocytes: Including monocytes and macrophages, these cells engulf and digest pathogens. They are vital for clearing infections and presenting antigens to adaptive immunity.
Monocytes: These white blood cells differentiate into macrophages or dendritic cells upon entering tissues. They contribute to both innate and adaptive immune processes.
Macrophages: These phagocytic cells process antigens and present them to T cells, bridging innate and adaptive immunity. They are abundant in the palatine tonsil.
Adaptive Immunity: This specific, long-term immune response involves T and B lymphocytes. It develops memory cells to provide future protection against specific pathogens.
T memory cells: These long-lived cells “remember” previous infections, enabling a faster response upon re-exposure. They are crucial for adaptive immunity’s memory function.
T effector cells: These active T cells directly attack infected cells or coordinate immune responses. They play a key role in cell-mediated immunity.
B memory cells: These cells retain memory of specific antigens, enabling rapid antibody production upon re-infection. They enhance the adaptive immune response.
B effector cells: These plasma cells produce antibodies to neutralize pathogens. They are essential for humoral immunity within the germinal center.
Antibodies: Proteins secreted by B effector cells that bind to pathogens, marking them for destruction. They are a hallmark of adaptive immunity.
Germinal center of palatine tonsil: This region within the tonsil is where B cells proliferate and differentiate. It is a hub for generating memory and effector B cells.
T lymphocyte: These cells, including T memory and effector types, orchestrate adaptive immunity. They recognize antigens presented by macrophages or dendritic cells.
Antigen-presenting cells: These cells, such as macrophages, display antigens to T lymphocytes. They are critical for activating adaptive immune responses.
B lymphocytes: These cells differentiate into B memory and effector cells, producing antibodies. They are central to the humoral arm of adaptive immunity.
Anatomical Context of Immune Cooperation
The palatine tonsil serves as a frontline defender, integrating innate and adaptive immunity effectively.
- The palatine tonsil traps pathogens, initiating surface defenses like mucus and hair.
- Pathogens entering the nasal or oral cavity trigger innate responses, including histamine release.
- Internal defenses like macrophages and natural killer cells neutralize immediate threats.
- The germinal center within the tonsil fosters B lymphocyte maturation, producing antibodies.
- T lymphocytes coordinate cellular immunity, enhancing the adaptive response.
- Monocytes and phagocytes bridge the two systems, presenting antigens to activate T cells.
This anatomical setup ensures a seamless transition from innate to adaptive immunity.
Mechanisms of Innate Immunity
Innate immunity provides an immediate barrier against pathogens, setting the stage for adaptation.
- Skin and hair form physical barriers, trapping pathogens before they penetrate tissues.
- Mucus in the tonsil region captures microbes, aiding their removal via ciliary action.
- Mast cells release histamine, causing inflammation to recruit phagocytes.
- Natural killer cells target infected cells, providing early viral defense.
- The complement system enhances pathogen marking, boosting phagocyte efficiency.
- Monocytes differentiate into macrophages, engulfing pathogens in the tonsil.
This rapid response is crucial for containing infections until adaptive immunity engages.
Role of Adaptive Immunity in Tonsil Function
Adaptive immunity builds on innate efforts, offering specific and lasting protection.
- T lymphocytes recognize antigens, activating T memory and effector cells in the germinal center.
- Antigen-presenting cells, like macrophages, initiate T cell responses within the tonsil.
- B lymphocytes proliferate, differentiating into B memory and effector cells.
- Antibodies produced by B effector cells neutralize pathogens, enhancing immunity.
- T memory cells ensure long-term protection, recalling past infections efficiently.
- The germinal center supports this process, amplifying adaptive responses over time.
This targeted approach strengthens the tonsil’s role in sustained immunity.
Clinical Relevance of Immune Cooperation
Understanding this interplay aids in managing immune-related conditions.
- Inflamed tonsils may indicate overactive innate responses, such as excessive histamine release.
- Weak adaptive immunity can lead to recurrent tonsillitis, requiring medical evaluation.
- Phagocyte dysfunction may impair antigen presentation, affecting T cell activation.
- B lymphocyte deficiencies can reduce antibody production, increasing infection risk.
- Natural killer cell activity is key in assessing viral susceptibility.
- The germinal center’s health is critical in diagnosing lymphoid disorders.
This knowledge supports effective treatment strategies for tonsil-related issues.
The collaboration between innate and adaptive immunity, centered in the palatine tonsil, is a testament to the body’s sophisticated defense system. By leveraging surface barriers, internal phagocytes, and adaptive memory cells, the tonsil ensures comprehensive protection, making it a fascinating focus for exploring immune health and resilience.

