The image presents a detailed cross-section of bronchial asthma tissue, highlighting the structural changes associated with this chronic respiratory condition. This visual representation is invaluable for understanding the pathological alterations, such as thickened mucosa and increased immune cell presence, that occur during an asthma attack. It serves as a critical tool for delving into the complexities of bronchial asthma, offering insights into its impact on lung function.
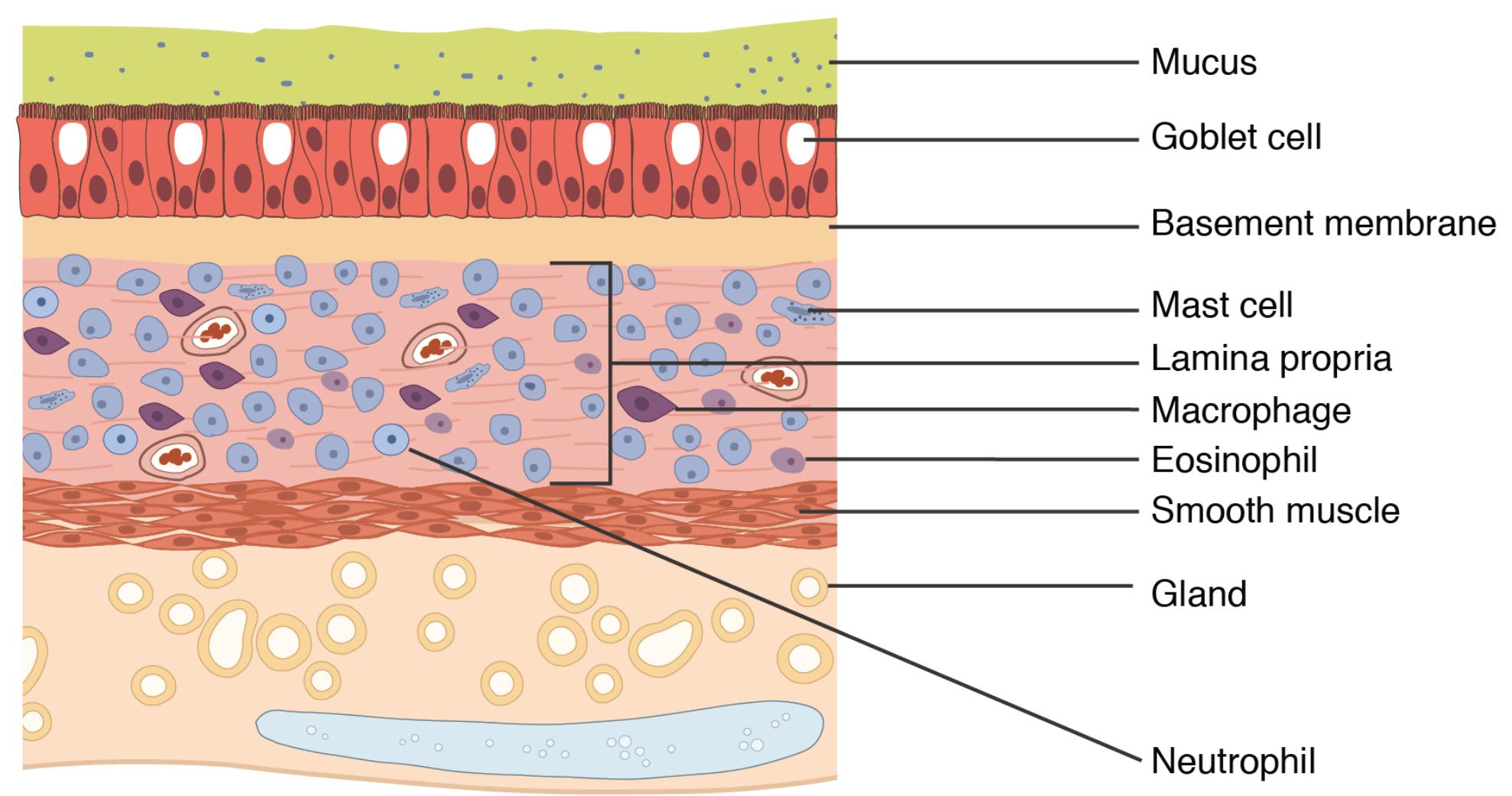
- Mucus: This layer appears thickened in bronchial asthma, trapping more debris and pathogens due to excessive production during an attack. It contributes to airway obstruction, making breathing difficult for affected individuals.
- Goblet cell: These cells are hyperactive in asthma, producing an increased amount of mucus that clogs the airways. Their proliferation is a key feature during an asthma exacerbation, exacerbating respiratory distress.
- Basement membrane: In asthma, this layer often thickens due to chronic inflammation, providing a scaffold for epithelial changes. It plays a role in the structural remodeling seen in asthmatic airways.
- Mast cell: These cells release histamine and other mediators during an asthma attack, triggering inflammation and bronchoconstriction. Their presence is a hallmark of the allergic response in asthma.
- Lamina propria: This layer shows increased cellularity in asthma, with infiltration of inflammatory cells like eosinophils. It supports the airway structure but becomes a site of immune activity during attacks.
- Macrophage: These immune cells are more abundant in asthmatic tissue, phagocytosing debris and contributing to the inflammatory response. They help modulate the immune environment but can perpetuate inflammation.
- Eosinophil: This cell type is significantly elevated in bronchial asthma, releasing toxic granules that damage airway tissue. Their infiltration is a defining characteristic of allergic asthma.
- Smooth muscle: The smooth muscle layer hypertrophies in asthma, leading to airway narrowing and increased resistance to airflow. This change is responsible for the wheezing heard during an attack.
- Gland: Glands in asthmatic tissue produce excess mucus, contributing to the thickened mucosal layer. Their hyperactivity worsens airway obstruction during asthma episodes.
- Neutrophil: These cells may increase during severe asthma attacks, contributing to acute inflammation and tissue damage. Their role is more prominent in non-allergic asthma variants.
Overview of Bronchial Asthma Tissue Anatomy
The bronchial asthma tissue depicted reveals significant deviations from normal lung structure, reflecting the disease’s impact. Each labeled component showcases adaptations that affect respiratory efficiency, making this image a key resource for study. Understanding these changes is essential for managing bronchial asthma effectively.
- The mucus layer’s thickening obstructs airways, a common symptom during asthma flares.
- Goblet cells overproduce mucus, leading to a viscous layer that hinders airflow.
- The basement membrane thickening supports chronic inflammation, a persistent feature in asthma.
- Mast cells initiate allergic responses, releasing mediators that constrict airways.
- The lamina propria becomes a battleground for immune cells, amplifying inflammation.
- Macrophages clear debris but also sustain the inflammatory cycle in asthma.
- Eosinophils drive allergic inflammation, damaging the airway epithelium.
- The smooth muscle hypertrophy increases airway resistance, a critical factor in asthma severity.
- Glands exacerbate mucus buildup, worsening breathing difficulties.
- Neutrophils contribute to acute inflammation, particularly in severe cases.
Pathophysiology of Bronchial Asthma
The pathophysiological changes in bronchial asthma tissue are driven by complex interactions among its layers. These alterations lead to the characteristic symptoms of wheezing, shortness of breath, and chest tightness. This section explores how each component contributes to the disease process.
- The mucus layer’s excess production clogs airways, reducing oxygen intake during attacks.
- Goblet cells respond to inflammatory triggers, over-secreting mucus as a protective mechanism.
- The basement membrane remodeling reflects long-term inflammation, altering airway mechanics.
- Mast cells release histamine, leukotrienes, and cytokines, initiating bronchoconstriction.
- The lamina propria hosts eosinophil and macrophage infiltration, sustaining chronic inflammation.
- Macrophages release pro-inflammatory cytokines, amplifying the immune response.
- Eosinophils release major basic protein, damaging epithelial cells and perpetuating asthma.
- The smooth muscle constriction narrows airways, a reversible process with treatment.
- Glands overactivity leads to mucus plugs, a common finding in asthma pathology.
- Neutrophils dominate in acute exacerbations, releasing enzymes that degrade tissue.
Clinical Implications and Management
The structural changes in bronchial asthma tissue have significant clinical relevance, guiding diagnosis and treatment strategies. Recognizing these alterations helps in tailoring therapies to alleviate symptoms and prevent exacerbations. This understanding is crucial for improving patient outcomes.
- The mucus buildup requires bronchodilators and mucolytics to clear airways effectively.
- Goblet cell hyperactivity may be managed with anti-inflammatory medications like corticosteroids.
- The basement membrane thickening indicates a need for long-term control with inhaled steroids.
- Mast cell stabilization can be achieved with antihistamines or mast cell inhibitors.
- The lamina propria inflammation responds to immunosuppressive therapies in severe cases.
- Macrophages modulation may involve anti-inflammatory agents to reduce cytokine release.
- Eosinophils levels guide biologic therapies like anti-IL-5 treatments for severe asthma.
- The smooth muscle response is targeted with bronchodilators like albuterol for quick relief.
- Glands overproduction may be controlled with anticholinergic drugs to reduce mucus.
- Neutrophils involvement suggests the need for systemic steroids in acute attacks.
The image of bronchial asthma tissue provides a window into the disease’s anatomical and physiological impact. These changes, from thickened mucus to eosinophil infiltration, underscore the need for comprehensive management strategies. By studying this structure, one can better appreciate the challenges of asthma and the importance of personalized treatment plans to enhance respiratory health.

