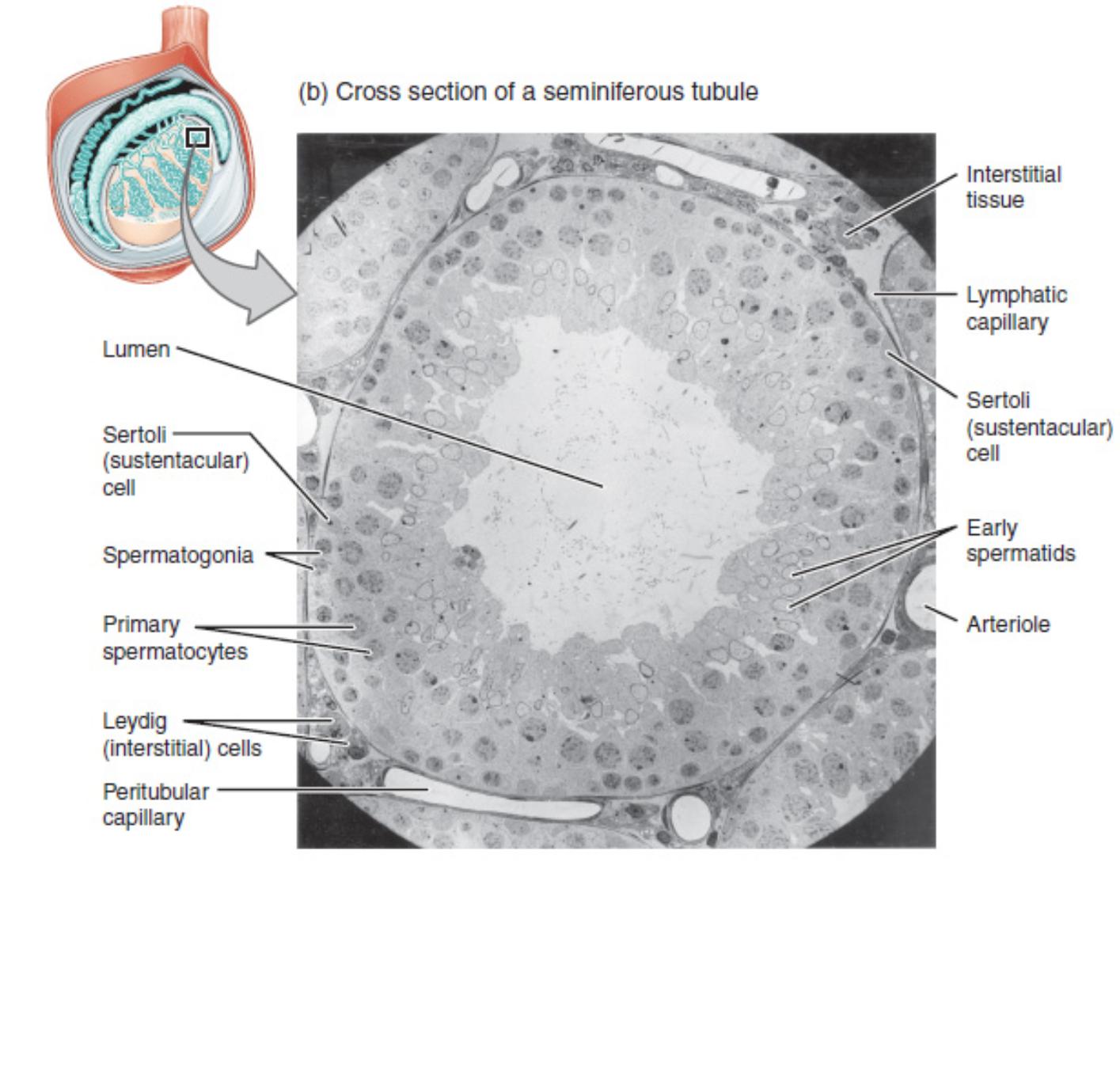
This article offers a detailed examination of a cross-section of a seminiferous tubule, as captured by an electron micrograph. The intricate cellular arrangement and specialized structures within these tubules are fundamental to male reproductive physiology, particularly the process of spermatogenesis. We will explore each labeled component, elucidating its anatomical features and physiological role in the production and maturation of sperm. This microscopic view provides invaluable insight into the highly organized environment essential for male fertility.
Anatomical Labels and Explanations:
Interstitial tissue: This refers to the connective tissue space located between adjacent seminiferous tubules within the testes. It houses various cell types, prominently including Leydig cells, which are critical for steroidogenesis.
Lymphatic capillary: These delicate vessels are part of the lymphatic system, responsible for collecting excess interstitial fluid and immune surveillance. Their presence in the interstitial tissue highlights the dynamic fluid environment surrounding the tubules.
Sertoli (sustentacular) cell: These are large, supportive cells that extend from the basement membrane towards the lumen of the seminiferous tubule. They play a crucial role in nourishing developing germ cells, forming the blood-testis barrier, and secreting factors essential for spermatogenesis.
Early spermatids: These are haploid germ cells that have completed meiosis II and are undergoing spermiogenesis, the final stage of maturation. They are characterized by their location closer to the lumen and the initiation of morphological changes into mature spermatozoa.
Arteriole: A small artery that provides oxygenated blood to the surrounding tissues, including the seminiferous tubule and the interstitial tissue. It is a key component of the vascular supply ensuring metabolic support for the active process of spermatogenesis.
Lumen: This is the central cavity within the seminiferous tubule, which appears as a light-shaded area in the micrograph. It serves as the space where mature spermatozoa are released before their transit out of the testis.
Spermatogonia: These are diploid stem cells located at the periphery of the seminiferous tubule, adjacent to the basement membrane. They are the foundational cells that undergo mitosis to maintain their population and produce primary spermatocytes.
Primary spermatocytes: These are diploid germ cells that have entered the first meiotic division (Meiosis I). They are typically larger than spermatogonia and are found deeper within the tubule wall, undergoing genetic recombination.
Leydig (interstitial) cells: Situated within the interstitial tissue, these endocrine cells are responsible for synthesizing and secreting androgens, predominantly testosterone. Testosterone is vital for the regulation of spermatogenesis and the development of male secondary sexual characteristics.
Peritubular capillary: These are small blood vessels that run alongside the seminiferous tubules. They facilitate the exchange of nutrients, hormones, and waste products between the bloodstream and the cells within the tubule, crucial for maintaining the delicate microenvironment required for sperm development.
The Seminiferous Tubule: A Microscopic Factory of Spermatogenesis
The electron micrograph presented offers a high-resolution glimpse into the complex architecture of a seminiferous tubule, the primary site of spermatogenesis in the male reproductive system. This image, sourced from a rat testis, beautifully illustrates the highly organized cellular arrangement that facilitates the continuous production of sperm. The lumen, visible as the central clear area, is the destination for developing germ cells.
The cellular layers radiating from the basement membrane towards the lumen represent distinct stages of sperm development.
- Spermatogonia are positioned at the very base, acting as stem cells.
- Moving inwards, primary spermatocytes are observed, engaged in the lengthy process of meiosis I.
- Further towards the lumen, early spermatids are undergoing spermiogenesis, transforming into their final, motile form.
- Throughout these stages, the large, supportive Sertoli cells provide structural integrity, nourishment, and crucial signaling molecules, forming the essential blood-testis barrier that protects the delicate developing germ cells.
The surrounding interstitial tissue is equally vital, housing Leydig cells which produce testosterone, the primary androgen necessary for the initiation and maintenance of spermatogenesis. This hormonal support, coupled with the rich vascular supply from arterioles and peritubular capillaries, ensures that the seminiferous tubule operates as an efficient biological factory. The coordinated function of these diverse cell types and structures underscores the elegance and precision of male reproductive physiology.
Conclusion
This electron micrograph of a seminiferous tubule provides a profound understanding of its intricate cellular landscape and the dynamic processes occurring within. Each labeled component plays a specific, indispensable role in the complex journey of spermatogenesis, from the initial germ cells to the final maturation of spermatozoa. The harmonious interaction between the structural support cells, the developing germ cells, and the endocrine environment of the interstitial tissue highlights the sophistication of the male reproductive system. A thorough grasp of this microscopic anatomy and its associated physiology is essential for comprehending male reproductive health and potential pathologies affecting fertility.

