This article presents a detailed analysis of a Doppler ultrasound scan taken from the right leg of a 65-year-old male patient presenting with significant swelling. The image clearly highlights the physiological and anatomical differences between patent blood vessels and those obstructed by pathology. We will examine the specific radiological signs of Deep Vein Thrombosis (DVT) in the subsartorial vein, contrasting the absence of blood flow in the thrombosed vessel against the healthy flow observed in the adjacent femoral artery and deep femoral vein.
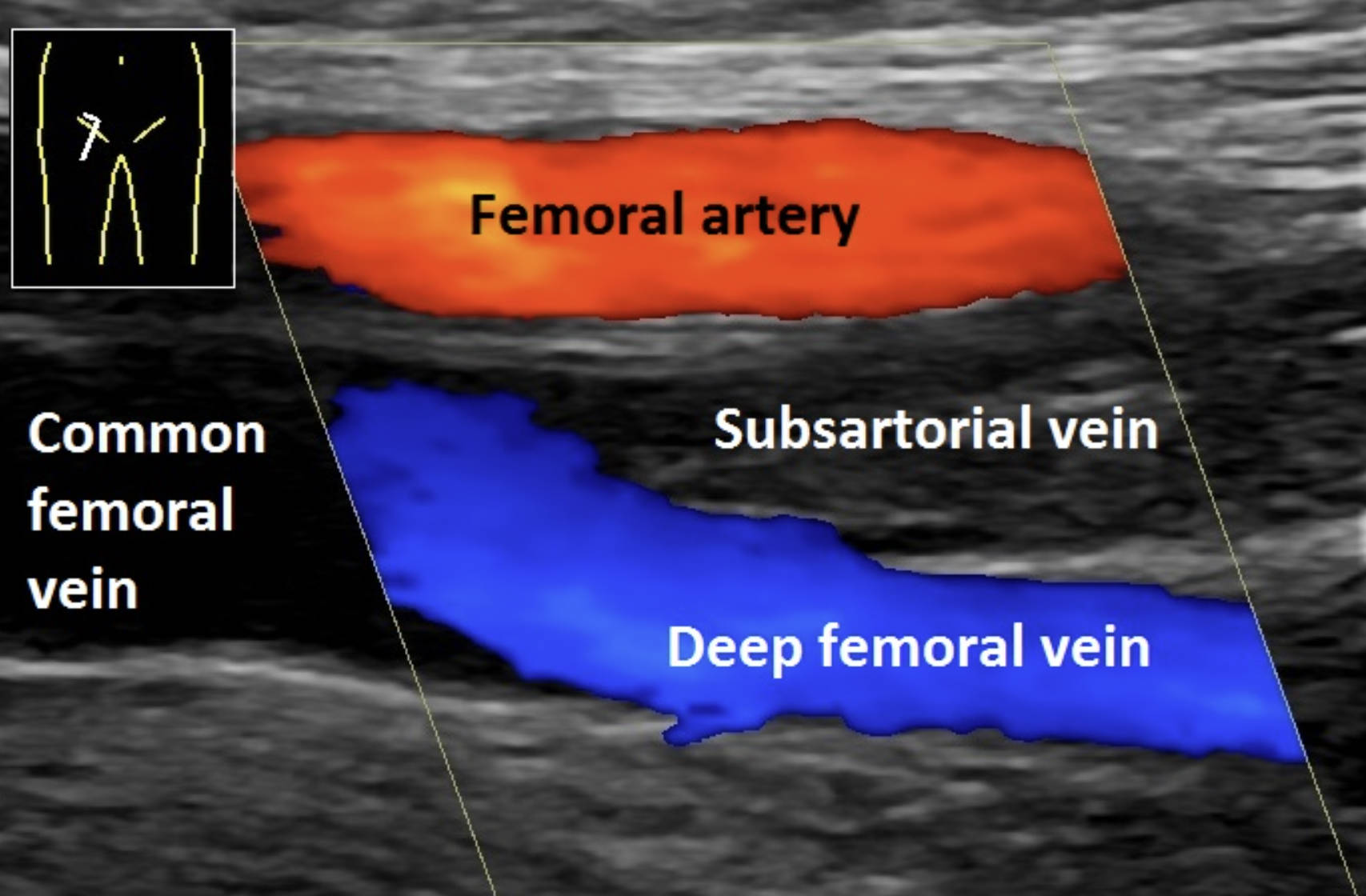
Femoral artery: This large blood vessel is depicted in red, indicating high-velocity oxygenated blood flowing towards the ultrasound probe. It serves as the primary arterial supply to the lower limb and remains fully patent in this scan, showing no signs of obstruction or narrowing.
Common femoral vein: Located to the left of the image, this is the major vein that receives blood from the deep femoral and femoral veins. In a standard ultrasound assessment, this vessel is typically compressed to check for clots, as it serves as the main conduit for venous return from the leg to the pelvis.
Subsartorial vein: This label identifies the affected vessel located within the adductor (subsartorial) canal, which shows no color signal. The lack of blue coloration indicates a complete absence of blood flow due to an obstruction, and the internal greyish appearance (hyperechogenicity) confirms the presence of a solid thrombus.
Deep femoral vein: Depicted in blue, this vein drains the deep muscles of the thigh and joins the femoral vein. The distinct blue color demonstrates that this vessel is patent and healthy, with deoxygenated blood flowing away from the probe as expected.
Principles of Vascular Ultrasound and Clot Detection
Doppler ultrasonography is the gold standard imaging modality for diagnosing venous thromboembolism in the lower extremities. This technology utilizes sound waves to visualize anatomical structures while simultaneously measuring the speed and direction of blood flow. In the provided image, color flow mapping is used: red typically represents flow towards the transducer (arterial), while blue represents flow away from the transducer (venous). When a vessel contains a blockage, such as a blood clot, the color signal is abruptly cut off or entirely absent, leaving a dark or grey void within the vessel walls.
The scan of this 65-year-old patient reveals a textbook case of venous obstruction. While the arterial system (red) is functioning correctly, the venous system is compromised. The presence of the clot in the subsartorial vein—a segment of the femoral vein running through the thigh’s adductor canal—explains the patient’s symptoms. When venous return is blocked, blood pools in the extremity, leading to hydrostatic pressure imbalances that force fluid into the surrounding tissues, resulting in the visible swelling and edema associated with the condition.
The diagnostic criteria for DVT on an ultrasound include several specific findings visible here and in dynamic testing:
- Absence of color flow: As seen in the subsartorial vein, blood cannot move through the clot.
- Non-compressibility: A healthy vein collapses when pressed with the probe; a thrombosed vein remains round and rigid.
- Hyperechogenicity: Over time, clots become denser and reflect more sound waves, appearing brighter (grey/white) than flowing blood.
- Venous distension: The blocked vein often appears larger than the accompanying artery due to trapped blood.
Pathophysiology of Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) is a serious medical condition involving the formation of a thrombus (blood clot) within the deep venous system. The pathophysiology is often described by Virchow’s Triad, which outlines three factors contributing to thrombosis: stasis of blood flow, endothelial injury (damage to the vein wall), and hypercoagulability (increased tendency to clot). In older adults, factors such as reduced mobility, underlying malignancies, or cardiovascular disease can precipitate stasis, leading to clot formation in the large veins of the thigh or calf.
In the case presented, the thrombus is located in the subsartorial region. The lack of flow indicated by the Doppler void suggests a significant occlusion. As the clot matures, it transforms from a soft, dark mass into a firmer, brighter structure on the screen—a characteristic noted as hyperechogenicity in the annotated image. If left untreated, the thrombus can propagate proximally into the common femoral vein or iliac veins, further compromising venous return and increasing the risk of long-term damage to the venous valves, known as post-thrombotic syndrome.
Clinical Risks and Management
The most critical and immediate risk associated with a DVT in the femoral system is a pulmonary embolism (PE). This occurs if a portion of the clot breaks loose (embolizes), travels through the inferior vena cava and the right side of the heart, and lodges in the pulmonary arteries of the lungs. A large PE can be fatal. Therefore, identifying a clot in a proximal vein like the subsartorial or femoral vein is a medical emergency requiring prompt intervention.
Treatment protocols generally focus on anticoagulation therapy. Medications such as heparin, warfarin, or Direct Oral Anticoagulants (DOACs) are administered to prevent the clot from growing and to stop new clots from forming. This allows the body’s natural fibrinolytic system to slowly degrade the existing thrombus over time. In severe cases where the clot burden is massive or the patient cannot take blood thinners, an inferior vena cava (IVC) filter may be placed to mechanically trap emboli before they reach the lungs.
Conclusion
The Doppler ultrasound image serves as a definitive diagnostic tool, clearly distinguishing between the healthy, flowing blood of the deep femoral vein and the obstructed, silent lumen of the thrombosed subsartorial vein. For the 65-year-old patient, this scan confirms the cause of leg swelling and dictates an immediate course of anticoagulant therapy. By visualizing the absence of flow and the texture of the clot, clinicians can assess the severity of the DVT and take necessary steps to prevent life-threatening complications.

