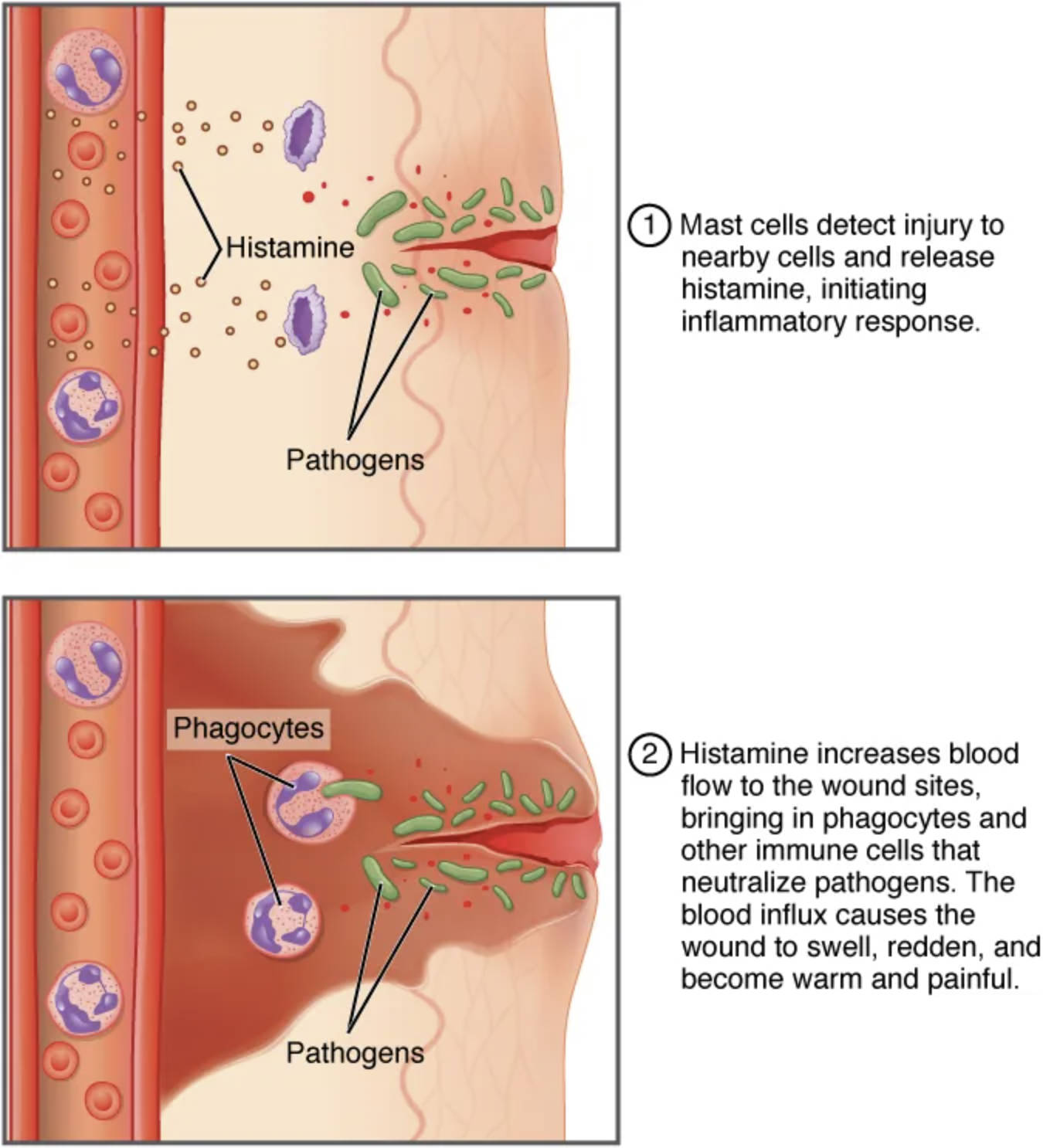
The inflammatory response is a fundamental defense mechanism that protects the body from injury and infection, manifesting as warmth, redness, pain, and swelling. Triggered by tissue damage or pathogen invasion, this process recruits phagocytes to eliminate threats and initiate healing, playing a critical role in maintaining health. This illustration provides a detailed view of the stages and components involved, offering insight into how the body orchestrates this vital reaction.
Labeled Components of the Inflammatory Response
Pathogen: This invading microorganism, such as bacteria or viruses, triggers the inflammatory response upon breaching the body’s barriers. It prompts the release of signaling molecules to alert the immune system.
Injured tissue: Damaged cells release chemicals like histamine and cytokines, initiating inflammation to isolate the injury. This area becomes the focal point for immune cell recruitment and repair.
Blood vessel: These vessels dilate and become more permeable during inflammation, allowing immune cells and fluids to reach the affected site. This contributes to redness and swelling in the region.
Histamine: Released by mast cells, histamine causes blood vessel dilation and increased permeability. It is a key mediator that leads to the classic signs of inflammation.
Cytokines: These signaling proteins, released by injured cells and immune cells, amplify the inflammatory response. They recruit phagocytes and coordinate the immune reaction.
Mast cells: Located near blood vessels, these cells release histamine and other mediators upon activation. They play an early role in initiating and sustaining inflammation.
Phagocytes: Including neutrophils and macrophages, these cells engulf and destroy pathogens and debris at the injury site. They are critical for clearing infections and promoting healing.
Neutrophils: The first phagocytes to arrive, neutrophils rapidly respond to inflammation by engulfing pathogens. They release enzymes to break down invaders, aiding in the acute phase.
Macrophages: These longer-acting phagocytes clean up debris and present antigens to adaptive immune cells. They contribute to both inflammation and tissue repair.
Fluid: Increased vascular permeability allows fluid to leak into tissues, causing swelling. This fluid also delivers nutrients and oxygen to support healing.
Redness: Resulting from blood vessel dilation, redness is a visible sign of increased blood flow to the inflamed area. It reflects the body’s effort to deliver immune cells.
Warmth: Generated by enhanced blood flow and metabolic activity, warmth indicates active inflammation. It helps create an environment less favorable to some pathogens.
Swelling: Caused by fluid accumulation and immune cell infiltration, swelling protects the injury by immobilizing it. It also signals the extent of the inflammatory response.
Pain: Arising from pressure on nerves due to swelling and the release of pain mediators, pain alerts the body to the injury. It encourages rest to facilitate recovery.
Anatomical Context of Inflammation
Inflammation occurs across various tissues, with blood vessels and immune cells playing central roles.
- Pathogens or injured tissue trigger the release of histamine and cytokines.
- Blood vessels dilate, increasing blood flow and permeability to deliver phagocytes.
- Mast cells activate near the injury, releasing mediators to amplify the response.
- Phagocytes like neutrophils and macrophages target the affected area.
- Fluid leakage contributes to swelling, supporting immune cell movement.
- Redness and warmth reflect heightened vascular and metabolic activity.
This illustration showcases the localized nature of the inflammatory response.
Physiological Mechanisms of Inflammation
The body employs a coordinated approach to manage inflammation effectively.
- Histamine and cytokines signal blood vessels to dilate, enhancing immune cell delivery.
- Neutrophils arrive quickly, engulfing pathogens within hours of injury.
- Macrophages follow, clearing debris and coordinating with adaptive immunity.
- Fluid accumulation provides a medium for immune cell migration and nutrient supply.
- Pain and swelling limit movement, protecting the injured site.
- Warmth and redness indicate active immune engagement against pathogens.
This process ensures rapid containment and resolution of damage.
Role of Phagocytes in Inflammation
Phagocytes are the workhorses of the inflammatory response, driving pathogen clearance.
- Neutrophils release antimicrobial substances, targeting bacteria at the injury site.
- Macrophages engulf larger debris, preventing secondary infections.
- Both cell types release cytokines, sustaining the inflammatory signal.
- Phagocytes present antigens, bridging innate and adaptive immunity.
- Their activity reduces tissue burden, aiding repair processes.
- Macrophages transition to a healing role as inflammation subsides.
This dual action highlights their versatility in immune defense.
Clinical Relevance of the Inflammatory Response
Understanding inflammation aids in managing related health conditions.
- Excessive inflammation can lead to chronic conditions like arthritis, causing persistent pain.
- Insufficient response may indicate immunodeficiency, increasing infection risk.
- Neutrophil overactivity can contribute to tissue damage in severe infections.
- Macrophage dysfunction may delay healing, prolonging swelling.
- Monitoring redness and warmth helps assess infection severity.
- Pain management strategies target mediators like histamine to reduce discomfort.
This knowledge supports effective diagnosis and treatment planning.
Regulation and Resolution of Inflammation
The body carefully regulates inflammation to prevent excessive damage.
- Cytokines signal the end of the acute phase, reducing phagocyte recruitment.
- Blood vessel permeability decreases as the threat subsides, limiting fluid leakage.
- Macrophages switch to an anti-inflammatory role, promoting tissue repair.
- Neutrophils undergo apoptosis, cleared by macrophages to end the response.
- Pain and swelling gradually resolve as healing progresses.
- Warmth diminishes with restored normal blood flow and metabolism.
This resolution ensures tissue integrity is maintained post-inflammation.
The inflammatory response, as depicted in this illustration, is a remarkable process that safeguards the body from harm through warmth, redness, pain, and swelling. By recruiting phagocytes and coordinating immune efforts, it exemplifies the body’s ability to heal and protect, offering a compelling area of study for those interested in human physiology.

