This diagram provides a clear and comprehensive illustration of Coronary Artery Bypass Graft (CABG) surgery, a vital procedure designed to restore adequate blood flow to the heart muscle. The image highlights the key anatomical structures involved and demonstrates how grafts are used to bypass critical blockages in the coronary arteries. Understanding the mechanics of CABG, as depicted, is crucial for patients and healthcare providers alike to appreciate its role in treating advanced coronary artery disease.
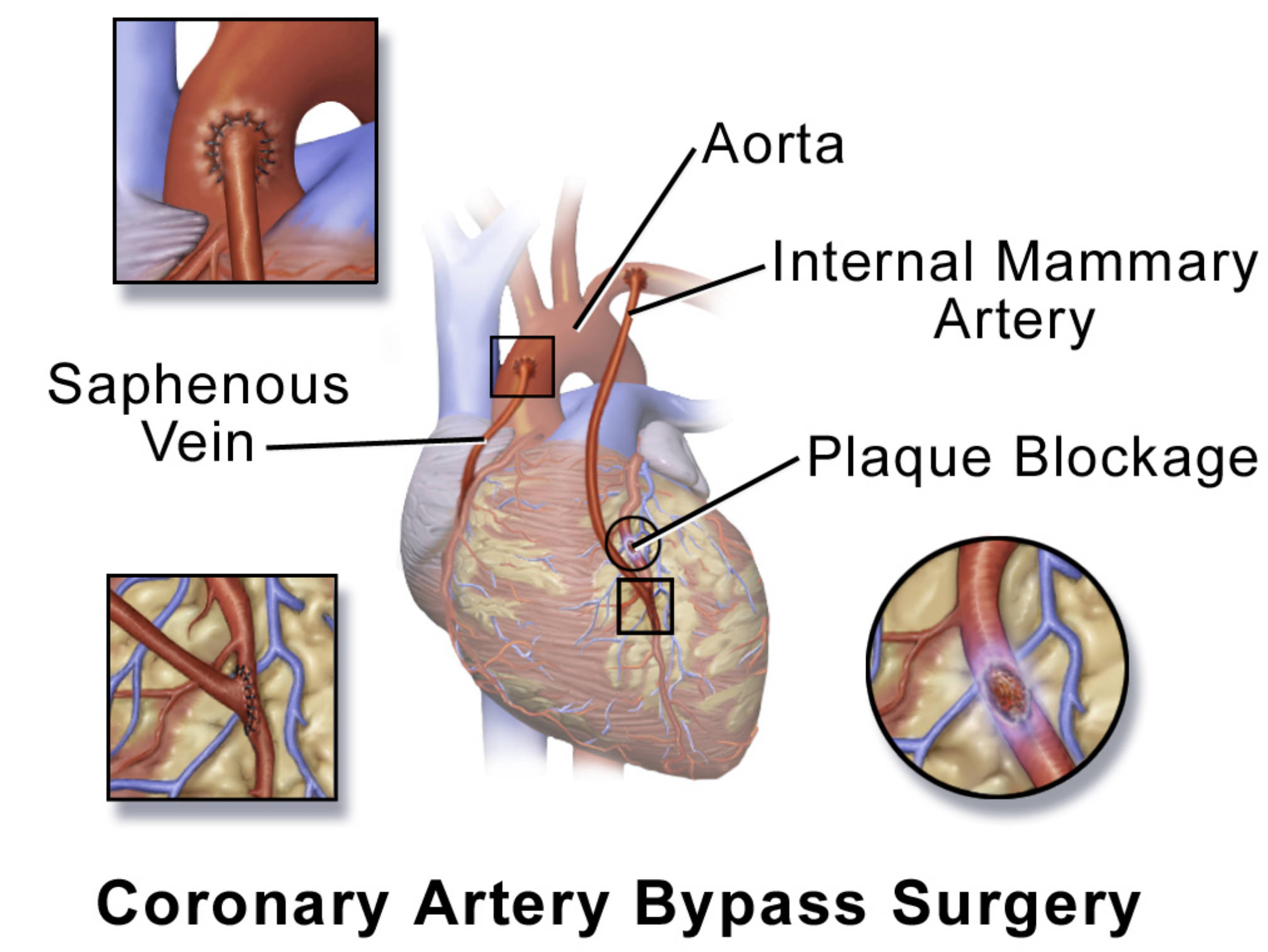
Aorta: The aorta is the largest artery in the body, originating from the left ventricle of the heart and extending down to the abdomen. In CABG surgery, the aorta serves as the main source of oxygenated blood to which one end of the bypass graft is typically attached. This connection ensures that the newly created bypass receives a direct supply of healthy blood for delivery to the heart muscle.
Internal Mammary Artery: The internal mammary artery, also known as the internal thoracic artery, is a major artery located in the chest wall. It is one of the most commonly used and preferred conduits for bypass grafts due to its excellent long-term patency rates. Its direct connection to the subclavian artery allows it to be used as a “pedicled” graft, meaning it remains attached at its origin and is simply swung down and anastomosed distal to the coronary blockage.
Saphenous Vein: The saphenous vein, usually harvested from the leg, is another frequently used vessel for bypass grafts. Segments of this vein are removed, reversed (because valves in veins prevent backward flow), and then used to create bypasses. One end is typically attached to the aorta and the other to the coronary artery beyond the blockage.
Plaque Blockage: This label points to an area within a coronary artery where there is a significant accumulation of plaque. This plaque, a hallmark of atherosclerosis, narrows the artery and severely restricts blood flow to the heart muscle. The purpose of CABG is to bypass this specific blockage, ensuring that the heart muscle receives the necessary oxygen and nutrients.
Introduction to Coronary Artery Bypass Graft (CABG) Surgery
Coronary Artery Bypass Graft (CABG) surgery is a major surgical procedure performed to treat severe coronary artery disease (CAD), a condition where the arteries supplying blood to the heart muscle become narrowed or blocked by plaque buildup. When these blockages significantly restrict blood flow, they can lead to symptoms like angina (chest pain), shortness of breath, and an increased risk of heart attack. CABG surgery aims to alleviate these symptoms and improve heart function by creating new pathways for blood to flow around the obstructed sections of the coronary arteries. The diagram vividly illustrates this process, showing how healthy blood vessels are used as grafts to bypass the blockages, thereby restoring optimal blood supply to the myocardium.
This intricate procedure involves harvesting healthy blood vessels from other parts of the patient’s body, such as the leg (saphenous vein) or the chest (internal mammary artery), and then surgically attaching them to the coronary arteries, effectively bypassing the diseased segments. The result is improved oxygenation of the heart muscle, leading to symptom relief, enhanced exercise tolerance, and potentially a prolonged lifespan. CABG is often considered for patients with multiple vessel disease, complex blockages, or those who have not responded well to less invasive treatments like angioplasty and stenting.
The decision to proceed with CABG is made after a thorough evaluation by a cardiology team, considering the extent of the blockages, the patient’s overall health, and other risk factors. This surgery represents a significant intervention, typically performed under general anesthesia, often involving a heart-lung machine that temporarily takes over the functions of the heart and lungs. However, advancements in surgical techniques also allow for “off-pump” or “beating-heart” bypass surgery in selected cases.
Key indications for Coronary Artery Bypass Graft (CABG) surgery include:
- Multiple coronary artery blockages: Especially in major arteries.
- Severe narrowing of the left main coronary artery: As this artery supplies a large portion of the heart.
- Blockages not amenable to percutaneous coronary intervention (PCI): Such as very long or calcified lesions.
- Diabetes mellitus with multi-vessel CAD: CABG often provides superior outcomes in this patient group.
- Persistent angina despite medical therapy: When symptoms significantly impact quality of life.
- Emergent situations: Such as after a severe heart attack with ongoing ischemia.
These factors guide the decision-making process for surgical intervention.
The Pathophysiology of Coronary Artery Disease
Coronary artery disease (CAD) is predominantly caused by atherosclerosis, a progressive process where fatty deposits, cholesterol, calcium, and other substances accumulate to form plaques within the inner lining of the coronary arteries. These arteries are crucial as they deliver oxygen-rich blood to the heart muscle (myocardium). As plaques grow, they narrow the arterial lumen, reducing blood flow. This restriction in blood supply, known as ischemia, deprives the heart muscle of the oxygen it needs to function properly.
When the heart muscle experiences ischemia, it can manifest as angina, which is chest pain or discomfort. If a plaque ruptures, it can trigger the formation of a blood clot (thrombus) that can completely block the artery, leading to a myocardial infarction (heart attack). Over time, chronic ischemia can also weaken the heart muscle, leading to heart failure. The severity and location of these blockages dictate the best treatment approach. CABG becomes a necessary intervention when the blockages are extensive, critical, and cannot be adequately managed by less invasive means, as it offers a direct solution to re-establish robust blood flow beyond the obstructions.
The CABG Surgical Procedure
Coronary Artery Bypass Graft surgery involves creating new routes for blood to flow around blocked coronary arteries, effectively restoring blood supply to the heart muscle. The procedure typically begins with the harvesting of bypass grafts. As illustrated in the diagram, commonly used conduits include:
- Internal Mammary Artery (IMA): Often referred to as the “gold standard” graft, the left IMA is frequently used to bypass blockages in the left anterior descending (LAD) coronary artery. The IMA is carefully dissected from the chest wall but remains attached at its origin from the subclavian artery. Its free end is then connected (anastomosed) to the coronary artery beyond the blockage. Its natural arterial connection ensures excellent long-term patency.
- Saphenous Vein Graft (SVG): Segments of the saphenous vein are harvested from the leg. Because veins have valves that prevent backward blood flow, the harvested vein segment must be reversed before implantation or its valves must be destroyed. One end of the SVG is typically sewn to the aorta, and the other end is connected to the coronary artery distal to the blockage. Multiple vein grafts can be used to bypass several blocked arteries.
- Radial Artery: Less commonly, the radial artery from the arm can also be used as a bypass graft.
During the surgery, the patient is usually placed on a heart-lung machine (cardiopulmonary bypass) to temporarily take over the functions of the heart and lungs, allowing the surgeon to work on a still heart. Once the grafts are in place and successfully connected, the heart-lung machine is gradually weaned off, and the heart resumes beating. The chest is then closed, marking the completion of the procedure.
Recovery and Long-Term Outlook After CABG
Recovery from CABG surgery is a significant process that typically involves several days in the hospital, followed by a period of rehabilitation at home. Patients will experience pain and discomfort from the chest incision and any graft harvest sites, which are managed with medication. Cardiac rehabilitation programs are crucial during recovery, helping patients gradually regain strength, improve cardiovascular fitness, and make necessary lifestyle changes. These programs often include supervised exercise, dietary counseling, and education on risk factor management.
The long-term outlook after CABG surgery is generally excellent, with significant improvement in symptoms and quality of life for most patients. The relief of angina and improved heart function can allow patients to resume normal activities and enjoy a more active lifestyle. However, it is important to remember that CABG treats the effects of coronary artery disease but does not cure the underlying atherosclerosis. Therefore, lifelong adherence to a heart-healthy lifestyle, including a balanced diet, regular exercise, smoking cessation, and strict management of risk factors such such as high blood pressure, cholesterol, and diabetes, is essential to prevent new blockages in the native coronary arteries or the bypass grafts themselves. Regular follow-up with a cardiologist is also critical to monitor heart health and address any emerging issues.

