Patent ductus arteriosus (PDA) is a congenital heart condition where the ductus arteriosus, a fetal blood vessel, fails to close after birth, allowing abnormal blood flow between the aorta and pulmonary artery. This diagram illustrates the anatomical location and implications of this persistent opening, providing a visual guide to understanding its impact on the circulatory system. Exploring this image offers valuable insights into the condition’s effects and the importance of early intervention.
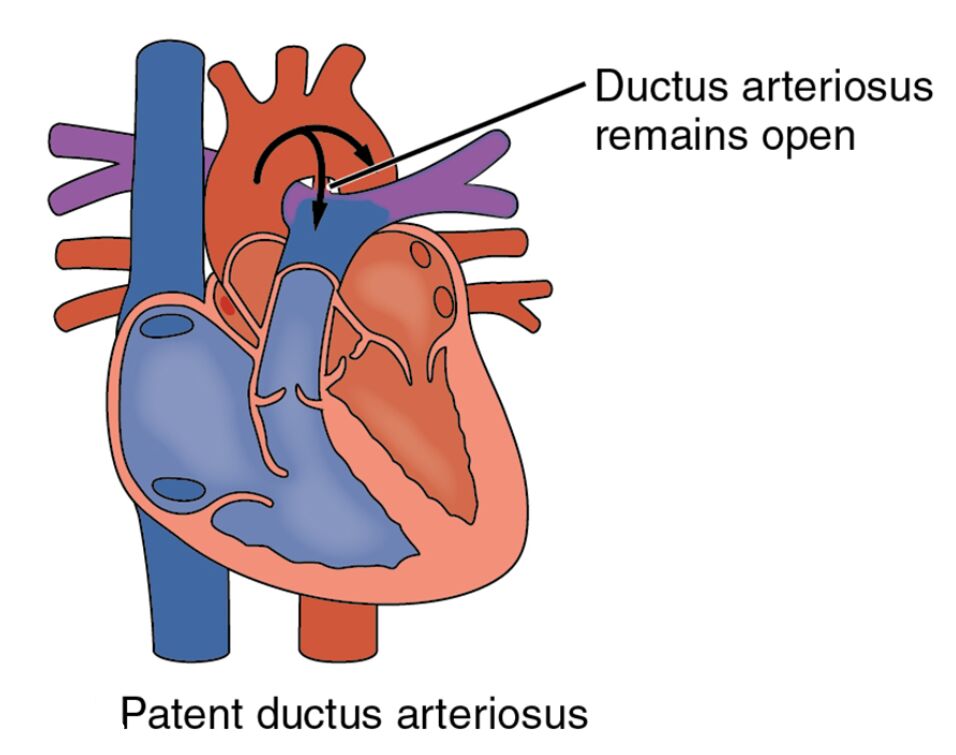
Pulmonary artery: The pulmonary artery carries deoxygenated blood from the right ventricle to the lungs for oxygenation, normally separated from the aorta after birth. In patent ductus arteriosus, this vessel remains connected to the aorta, leading to increased blood flow to the lungs.
Aorta: The aorta distributes oxygenated blood from the left ventricle to the rest of the body, serving as the main systemic artery. A patent ductus arteriosus causes a left-to-right shunt, where extra blood flows back into the pulmonary artery from the aorta.
Ductus arteriosus: The ductus arteriosus is a temporary fetal vessel that bypasses the lungs by connecting the pulmonary artery to the aorta, typically closing shortly after birth. When it fails to close, it results in patent ductus arteriosus, creating an abnormal circulatory pathway.
Anatomical Overview of Patent Ductus Arteriosus
The heart and major blood vessels undergo significant changes after birth, and this diagram highlights the normal and affected states in PDA. Recognizing the anatomy helps in understanding the defect’s physiological consequences.
- The pulmonary artery normally directs blood to the lungs, but in PDA, it receives excess flow from the aorta.
- The aorta’s role in systemic circulation is compromised by the shunt, increasing the heart’s workload.
- The ductus arteriosus’ persistence allows blood to recirculate, altering pulmonary and systemic pressures.
- This condition is more common in premature infants, reflecting developmental differences.
The diagram underscores the importance of postnatal vascular closure.
Physiological Impact and Symptoms
Patent ductus arteriosus disrupts normal blood flow, leading to a range of physiological effects. The image illustrates how this defect influences cardiovascular function.
- The pulmonary artery experiences increased pressure and volume, potentially causing pulmonary hypertension.
- The aorta’s left-to-right shunt can lead to a machinery-like heart murmur, detectable through a stethoscope.
- The ductus arteriosus’ open state forces the heart to pump more blood, risking heart failure over time.
- Symptoms like poor weight gain or shortness of breath may appear, especially in infants.
Echocardiography is the primary tool for diagnosing this condition.
Causes and Risk Factors
The development of patent ductus arteriosus involves genetic and environmental factors during fetal growth. Identifying these aids in prevention and management.
- Prematurity is a significant risk factor, as the ductus arteriosus may not mature fully before birth.
- Maternal rubella infection during pregnancy can contribute to congenital heart defects.
- Genetic predisposition, such as in certain chromosomal abnormalities, increases susceptibility.
- Prenatal monitoring with ultrasound can identify potential issues, guiding postnatal care.
Adequate prenatal care reduces the likelihood of related complications.
Diagnosis and Treatment Options
Diagnosing and managing patent ductus arteriosus requires a tailored approach based on the patient’s age and symptoms. Imaging and clinical assessment are key.
- Echocardiography visualizes the ductus arteriosus to assess the size and direction of the shunt.
- In premature infants, indomethacin or ibuprofen may promote closure of the ductus arteriosus.
- Surgical ligation or catheter-based closure is considered for larger or symptomatic cases.
- Regular follow-ups ensure the condition does not lead to long-term pulmonary damage.
Timely intervention improves outcomes significantly.
Clinical Relevance and Long-Term Outlook
Understanding the implications of patent ductus arteriosus is essential for long-term health management. The defect’s impact varies with its severity and treatment.
- The pulmonary artery’s overload can lead to irreversible lung changes if untreated.
- The aorta’s shunt may cause endocarditis risk, requiring prophylactic antibiotics.
- Successful closure of the ductus arteriosus restores normal circulation, enhancing quality of life.
- Adults with undiagnosed PDA may need monitoring for heart failure or pulmonary hypertension.
Lifestyle adjustments support cardiovascular health post-treatment.
Conclusion
This diagram of patent ductus arteriosus provides a detailed view of the pulmonary artery, aorta, and ductus arteriosus, illustrating the impact of this congenital heart defect on blood flow. By showing how the failure of the ductus arteriosus to close affects the heart and lungs, it emphasizes the need for early detection and appropriate management. This understanding equips individuals with the knowledge to address the challenges of PDA effectively, improving long-term health outcomes.

