The male reproductive system is an intricate network of organs and ducts designed for the production, maturation, and transport of sperm, as well as the synthesis of male sex hormones. This detailed lateral view diagram offers a crucial insight into the anatomical relationships of both internal and external structures. Understanding these components—from the primary gonads to the accessory glands and intricate duct system—is fundamental to comprehending male reproductive physiology, urinary function, and the clinical implications of various conditions.
Exploring the Structures of the Male Reproductive System
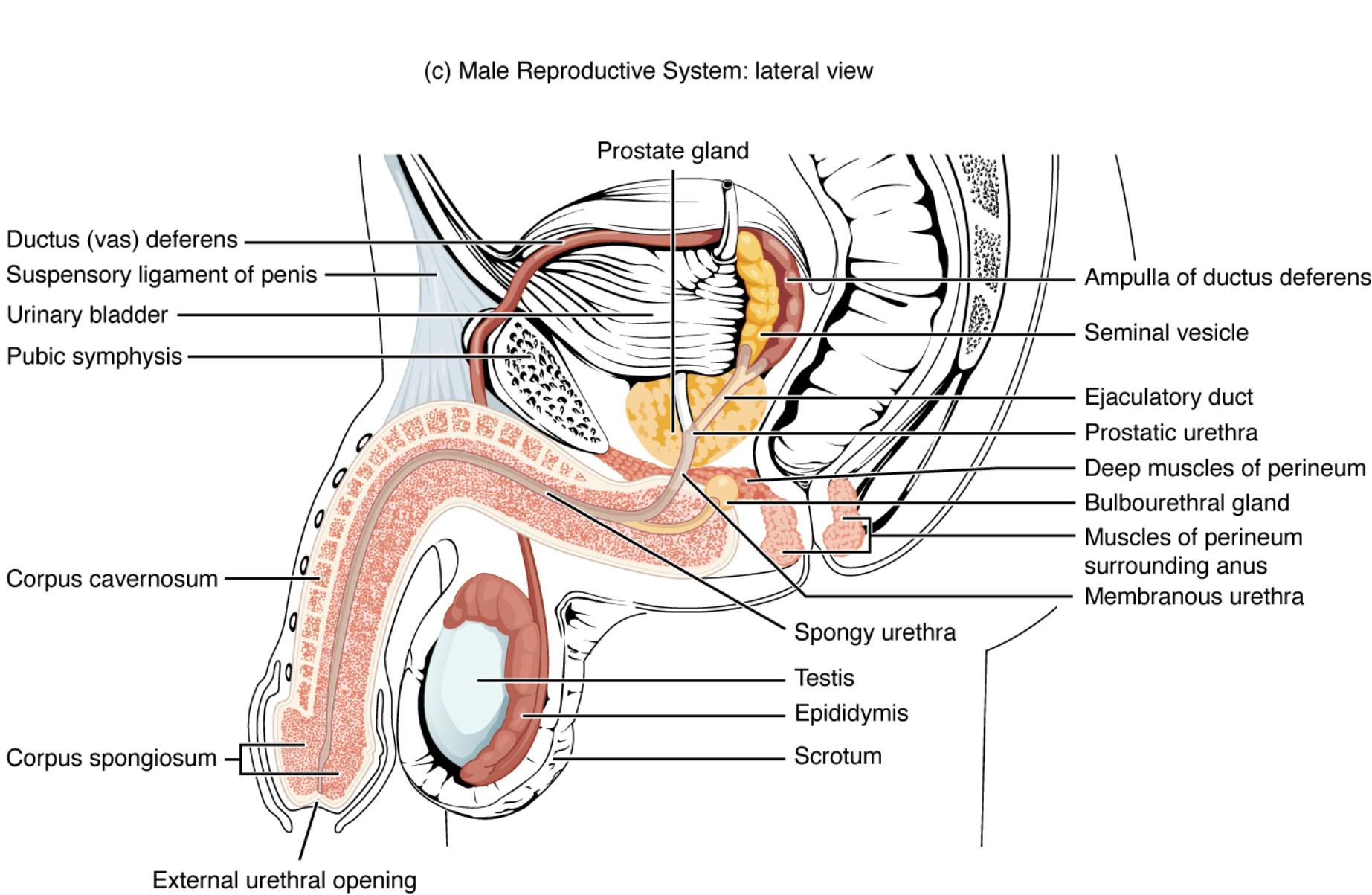
c) Male Reproductive System: lateral view: This comprehensive cross-sectional diagram provides a lateral internal view of the male reproductive organs, showcasing their anatomical relationships within the pelvic cavity and externally. It highlights the intricate network of ducts and glands involved in semen production and transport.
Ductus (vas) deferens: A muscular tube that transports sperm from the epididymis to the ejaculatory duct. It is a key component of the spermatic cord and contracts forcefully during ejaculation to propel sperm.
Suspensory ligament of penis: A fibrous band that extends from the pubic symphysis to the dorsal surface of the penis. It helps to support the weight of the penis and anchors it to the pelvis.
Urinary bladder: A muscular sac that stores urine received from the kidneys via the ureters. While part of the urinary system, its anatomical proximity and the passage of the urethra through the penis mean it is often visualized in diagrams of the male reproductive system.
Pubic symphysis: A cartilaginous joint located anteriorly between the two pubic bones of the pelvis. It provides a point of attachment for various pelvic structures, including the ligaments supporting the penis.
Corpus cavernosum: One of two large, dorsal columns of erectile tissue within the shaft of the penis. These spongy tissues fill with blood during sexual arousal, causing the penis to become erect.
Corpus spongiosum: A single, ventral column of erectile tissue within the penis, which surrounds the urethra. It helps to keep the urethra open during erection, preventing its compression.
External urethral opening: The distal opening of the urethra located at the tip of the glans penis. It serves as the exit point for both urine and semen.
Prostate gland: A walnut-sized gland located inferior to the urinary bladder and surrounding the prostatic urethra. It secretes a milky, slightly acidic fluid containing citrate (nutrient for sperm), enzymes, and prostate-specific antigen (PSA), contributing significantly to semen volume and viability.
Seminal vesicle: One of two sac-like glands located posterior to the urinary bladder. These glands secrete a yellowish, alkaline fluid rich in fructose (energy for sperm), prostaglandins, and clotting factors, accounting for about 60% of semen volume.
Ampulla of ductus deferens: The enlarged terminal portion of the ductus deferens, located just before it joins the seminal vesicle duct to form the ejaculatory duct. It serves as a temporary storage site for sperm prior to ejaculation.
Ejaculatory duct: Formed by the union of the ductus deferens ampulla and the seminal vesicle duct. It passes through the prostate gland and empties into the prostatic urethra, allowing sperm and seminal fluid to mix.
Prostatic urethra: The portion of the urethra that passes through the prostate gland. It receives ejaculatory ducts and ducts from the prostate gland.
Deep muscles of perineum: A group of muscles located in the pelvic floor, essential for supporting pelvic organs and playing a role in micturition and ejaculation.
Bulbourethral gland: Also known as Cowper’s gland, one of two small glands located inferior to the prostate gland, at the base of the penis. They secrete a clear, alkaline mucus into the spongy urethra before ejaculation, which lubricates the urethra and neutralizes any residual acidic urine.
Muscles of perineum surrounding anus: Refers to the muscles of the pelvic floor, including the external anal sphincter, which are crucial for continence and also support the pelvic organs.
Membranous urethra: The short, narrow portion of the urethra that passes through the deep muscles of the perineum. It connects the prostatic urethra to the spongy urethra.
Spongy urethra: The longest part of the urethra, extending through the corpus spongiosum of the penis to the external urethral opening. It transports urine and semen out of the body.
Testis: One of two oval-shaped male gonads located in the scrotum. The testes are responsible for spermatogenesis (sperm production) and the synthesis of male sex hormones, primarily testosterone.
Epididymis: A comma-shaped organ located posterior to each testis. It serves as a site for sperm maturation and storage, where sperm gain motility and the ability to fertilize an ovum.
Scrotum: A sac of skin and superficial fascia suspended inferior to the pubic symphysis and anterior to the anus. It contains the testes, epididymides, and the initial parts of the spermatic cords, maintaining a temperature suitable for spermatogenesis.
This detailed lateral view diagram provides an exceptional insight into the intricate anatomy of the male reproductive system. Far more than a collection of isolated organs, it illustrates a complex and interconnected network designed for the production, maturation, transport, and delivery of male gametes (sperm) and the synthesis of vital male sex hormones. From the primary gonads to the accessory glands and an elaborate duct system, each component plays a precise role in ensuring reproductive viability and overall physiological function.
The illustration highlights the deep anatomical relationships within the pelvic cavity and the external genitalia. Key structures such as the testes and epididymides, housed within the scrotum, are presented alongside the extensive duct system that includes the ductus (vas) deferens, ampulla, and ejaculatory ducts. These ducts serve as the sophisticated plumbing that guides sperm from their origin to the point of expulsion.
Crucially, the diagram also emphasizes the contributions of the accessory glands:
- The prostate gland, situated beneath the bladder, plays a significant role in semen volume and composition.
- The seminal vesicles, located posterior to the bladder, also contribute a substantial portion of the seminal fluid, providing nutrients and buffers essential for sperm survival.
- The bulbourethral glands, though small, add pre-ejaculate fluid that lubricates the urethra and neutralizes acidity.
The close anatomical relationship with the urinary system is also evident, particularly with the urinary bladder and the urethra passing through both the prostate gland and the penis. This shared pathway for urine and semen underscores the dual functionality of certain structures within the male urogenital system. Understanding these interconnections is vital for comprehending normal physiological processes, as well as for diagnosing and treating conditions that may affect male reproductive and urinary health.
Anatomy and Function of the Male Reproductive System
The male reproductive system is a remarkable biological apparatus essential for reproduction and the production of male hormones. This system is composed of primary and accessory organs, each with a specialized role in ensuring the viability and delivery of sperm. A comprehensive understanding of its anatomy and physiology is crucial for appreciating male health and fertility.
The primary reproductive organs are the testes, located within the scrotum, an external sac that provides a cooler environment vital for spermatogenesis (sperm production). Each testis is responsible for generating millions of sperm daily and for synthesizing androgens, primarily testosterone, which drives male secondary sexual characteristics and reproductive function. From the testes, immature sperm are transported to the epididymis, a highly coiled tube located posterior to each testis. Here, sperm undergo a crucial maturation process, gaining motility and the capacity to fertilize an ovum.
Following maturation, sperm are stored in the epididymis until ejaculation. During sexual arousal, sperm are propelled from the epididymis through the ductus deferens (also known as the vas deferens). Each ductus deferens extends superiorly into the pelvic cavity, loops over the urinary bladder, and widens to form the ampulla. The ampulla then joins with the duct of the seminal vesicle to form the ejaculatory duct. These ducts converge within the prostate gland, ultimately emptying into the prostatic urethra. Along this pathway, accessory glands contribute essential fluids to create semen.
The accessory glands include the seminal vesicles, prostate gland, and bulbourethral glands. The seminal vesicles secrete an alkaline fluid rich in fructose, a sugar that provides energy for sperm motility, along with prostaglandins and clotting factors. The prostate gland, situated inferior to the bladder, produces a milky, slightly acidic fluid containing citrate (another sperm nutrient), enzymes, and prostate-specific antigen (PSA), which helps to liquefy the semen after ejaculation. Finally, the bulbourethral glands secrete a clear, alkaline mucus prior to ejaculation, lubricating the urethra and neutralizing any residual acidic urine, thereby creating a more favorable environment for sperm passage. The combined secretions from these glands mix with sperm to form semen, a complex fluid designed to protect, nourish, and transport sperm effectively through the female reproductive tract. The semen is ultimately expelled from the body through the urethra, which traverses the length of the penis. The penis itself, composed of erectile tissues like the corpora cavernosa and corpus spongiosum, facilitates copulation through its ability to become erect upon sexual stimulation.
Conclusion
This detailed lateral view of the male reproductive system provides an invaluable foundation for understanding its complex anatomical arrangement and physiological functions. By meticulously illustrating the testes, epididymides, intricate duct system, and essential accessory glands, the diagram clarifies how sperm are produced, matured, and transported, and how semen is formed. A comprehensive grasp of these structures and their coordinated roles is crucial for comprehending male fertility, urinary health, and the diagnosis and treatment of various related conditions.

