Explore the various methods of pulmonary function testing, including spirometry and gas diffusion analysis, to understand how these diagnostic tools assess lung health. Learn about key measurements like Forced Vital Capacity (FVC), FEV1, and Total Lung Capacity (TLC), which are vital for diagnosing and managing respiratory conditions.
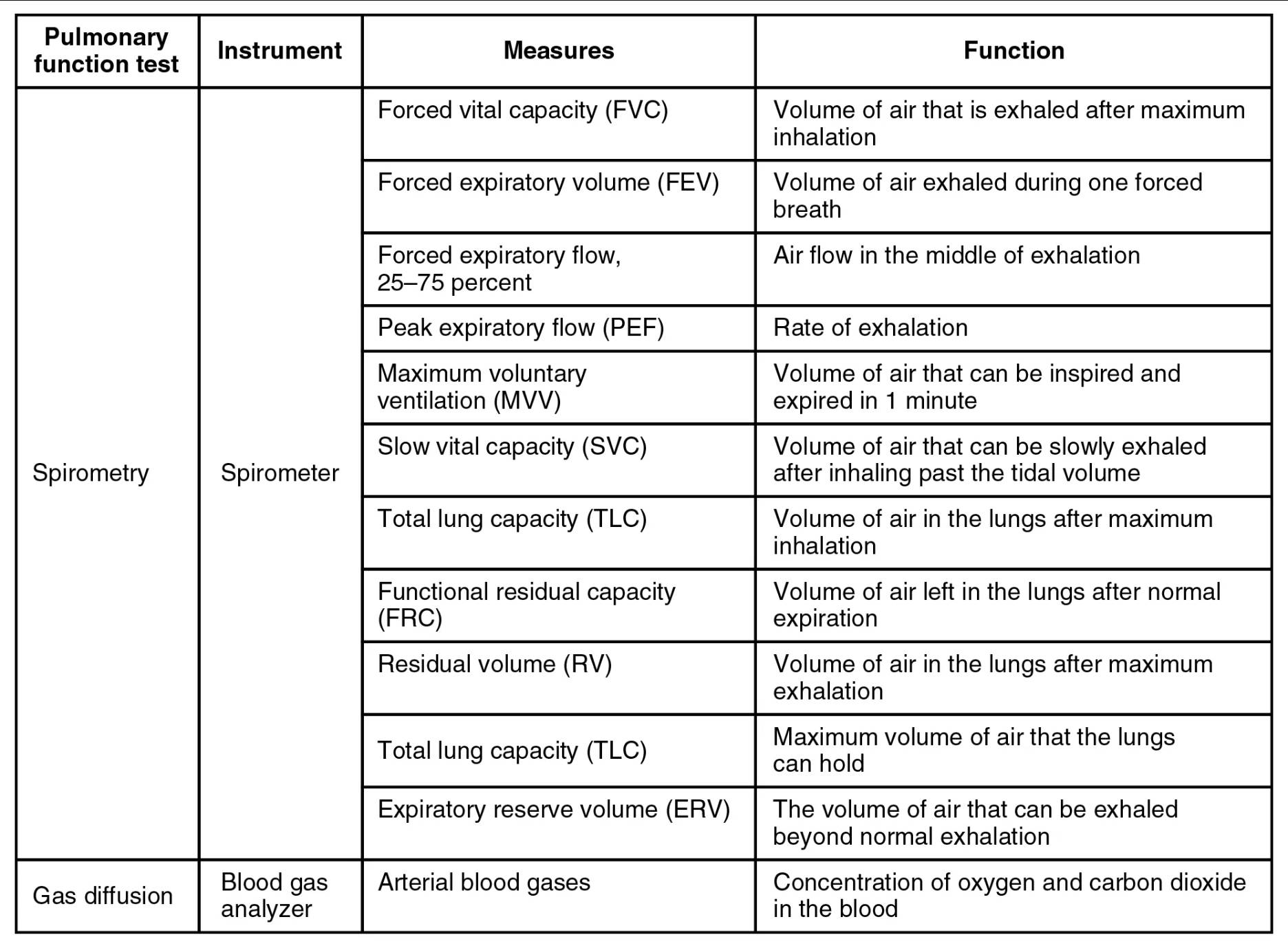
Pulmonary function test: These are a group of tests that measure how well your lungs are working. They assess lung volume, capacity, rates of flow, and gas exchange, providing critical information about respiratory health.
Spirometry: This is a common type of pulmonary function test that measures how much air you can inhale and exhale, and how quickly you can do so. It is performed using a spirometer and is crucial for diagnosing obstructive and restrictive lung diseases.
Spirometer: This is the instrument used to perform spirometry tests. Patients breathe into a mouthpiece connected to the device, which records various lung volumes and flow rates.
Forced vital capacity (FVC): This measures the total volume of air that can be exhaled forcibly and completely after a maximal inspiration. FVC is a fundamental indicator of lung function and is often reduced in both obstructive and restrictive lung diseases.
Forced expiratory volume (FEV): This specifically refers to the volume of air exhaled during one forced breath, typically within the first second (FEV1). A low FEV1, especially in relation to FVC, is a hallmark of obstructive lung diseases like asthma and COPD.
Forced expiratory flow, 25–75 percent (FEF25-75%): This measures the average flow rate of air during the middle portion of a forced exhalation. It is particularly sensitive to changes in the smaller airways and can detect early airway obstruction that FEV1 might miss.
Peak expiratory flow (PEF): This measures the maximum rate of exhalation achieved during a forced breath. PEF is a quick and simple measurement often used by patients with asthma to monitor their lung function at home.
Maximum voluntary ventilation (MVV): This measures the volume of air that can be inspired and expired in 1 minute with maximal effort. MVV assesses the overall strength of respiratory muscles and the elasticity of the lungs and chest wall.
Slow vital capacity (SVC): This is the volume of air that can be slowly exhaled after inhaling past the tidal volume. Unlike FVC, SVC is performed without forceful effort and can sometimes be larger than FVC in patients with severe airway obstruction.
Total lung capacity (TLC): This represents the maximum volume of air that the lungs can hold after a maximum inspiration. TLC is a comprehensive measure of lung size and is crucial for differentiating between restrictive and obstructive lung diseases.
Functional residual capacity (FRC): This is the volume of air left in the lungs after a normal expiration. FRC is important for maintaining oxygenation between breaths and is often increased in obstructive lung diseases due to air trapping.
Residual volume (RV): This is the volume of air that remains in the lungs after a maximum exhalation. RV cannot be exhaled and is essential for preventing alveolar collapse; it is typically elevated in conditions like emphysema.
Expiratory reserve volume (ERV): This refers to the volume of air that can be exhaled beyond normal exhalation. ERV reflects the additional air that can be expelled from the lungs after a quiet breath.
Gas diffusion: This refers to the process by which gases, specifically oxygen and carbon dioxide, move across the alveolar-capillary membrane in the lungs. Efficient gas diffusion is vital for effective oxygenation of the blood and removal of carbon dioxide.
Blood gas analyzer: This is an instrument used to measure the concentration of oxygen and carbon dioxide in the blood, along with blood pH. It provides critical information about the body’s acid-base balance and the efficiency of gas exchange.
Arterial blood gases: These are measurements of the partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2), as well as blood pH, in arterial blood. Arterial blood gases provide a direct assessment of the lung’s ability to oxygenate blood and remove carbon dioxide, crucial for evaluating respiratory failure.
Unveiling Lung Health: The Role of Pulmonary Function Testing
Pulmonary function tests (PFTs) are a group of diagnostic procedures designed to assess the efficiency and capacity of the lungs. These tests are invaluable tools for diagnosing various respiratory conditions, monitoring disease progression, and evaluating the effectiveness of treatments. By measuring how much air an individual can move in and out of their lungs, and how quickly, PFTs provide a detailed physiological snapshot of the respiratory system.
PFTs encompass a range of measurements, each offering unique insights into different aspects of lung function. The most common type of PFT is spirometry, which utilizes a spirometer to evaluate airflow mechanics. Beyond spirometry, other tests, such as gas diffusion analysis, provide critical information about the lungs’ ability to transfer oxygen into the bloodstream.
Key aspects assessed by PFTs include:
- Lung volumes and capacities
- Flow rates of air during breathing
- Efficiency of gas exchange
These comprehensive evaluations help differentiate between obstructive lung diseases, where airflow is hindered, and restrictive lung diseases, where lung expansion is limited.
Spirometry: A Cornerstone of Respiratory Diagnostics
Spirometry is a foundational pulmonary function test that measures how much air you can inhale, exhale, and how quickly you can do so. It is a non-invasive procedure, typically performed in a doctor’s office or clinic, where the patient breathes into a mouthpiece connected to a device called a spirometer. The resulting data helps healthcare providers assess lung health and diagnose conditions such as asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis.
Key Spirometric Measurements
Several crucial measurements are obtained during spirometry. Forced Vital Capacity (FVC) quantifies the total volume of air exhaled after a maximal inspiration. A reduced FVC can indicate either obstructive or restrictive lung disease. Forced Expiratory Volume in one second (FEV1) measures the volume of air exhaled during the first second of a forced breath. The FEV1/FVC ratio is particularly important; a low ratio is characteristic of obstructive lung diseases, indicating airflow limitation. Forced Expiratory Flow, 25-75% (FEF25-75%) assesses the average flow rate in the middle part of exhalation, which can reveal early small airway obstruction. Peak Expiratory Flow (PEF) represents the maximum speed of exhalation and is often used for daily monitoring by individuals with asthma. Maximum Voluntary Ventilation (MVV) evaluates the maximum amount of air that can be breathed in and out during a minute of forced breathing, reflecting overall respiratory muscle strength and endurance. Slow Vital Capacity (SVC) measures the volume of a slow, complete exhalation after a maximal inspiration, offering another perspective on lung volume.
Other significant spirometric values include Total Lung Capacity (TLC), which is the total volume of air the lungs can hold after a maximal inspiration. Functional Residual Capacity (FRC) measures the volume of air remaining in the lungs after a normal expiration, reflecting the resting volume. Residual Volume (RV) is the air that cannot be exhaled even after a maximal forced expiration, preventing alveolar collapse. Lastly, Expiratory Reserve Volume (ERV) is the additional amount of air that can be exhaled after a normal expiration. These detailed measurements collectively paint a comprehensive picture of an individual’s respiratory function, aiding in precise diagnosis and personalized treatment plans.
Gas Diffusion: Assessing the Lungs’ Exchange Efficiency
Beyond simply moving air in and out, the lungs’ primary role is to facilitate the exchange of gases: taking oxygen into the bloodstream and releasing carbon dioxide. Gas diffusion tests, often conducted using a blood gas analyzer, provide critical insights into this vital function. The Arterial Blood Gas (ABG) test measures the partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2) in arterial blood, along with blood pH. These values are crucial for assessing the efficiency of gas transfer across the alveolar-capillary membrane and identifying conditions such as hypoxemia (low oxygen in the blood) or hypercapnia (high carbon dioxide in the blood), which can be signs of respiratory failure. An ABG analysis is essential in critical care settings to monitor patients with acute respiratory distress, severe pneumonia, or other conditions affecting gas exchange.
Conclusion
Pulmonary function testing, encompassing both spirometry and gas diffusion analysis, stands as an indispensable diagnostic cornerstone in modern respiratory medicine. These tests provide invaluable quantitative data on lung volumes, flow rates, and the efficiency of gas exchange, enabling clinicians to accurately diagnose, stage, and monitor a wide spectrum of respiratory diseases. By leveraging these powerful tools, healthcare providers can tailor effective treatment strategies, ultimately improving patient outcomes and enhancing the understanding of respiratory health.

