This article explores the microscopic features of calcific atherosclerosis, a significant component of arterial disease, as illustrated by the provided image. We will delve into the anatomical layers of an artery and specifically examine the pathological changes associated with calcium deposition within atherosclerotic plaques. Understanding these intricate details is crucial for comprehending the progression and clinical implications of this widespread condition.
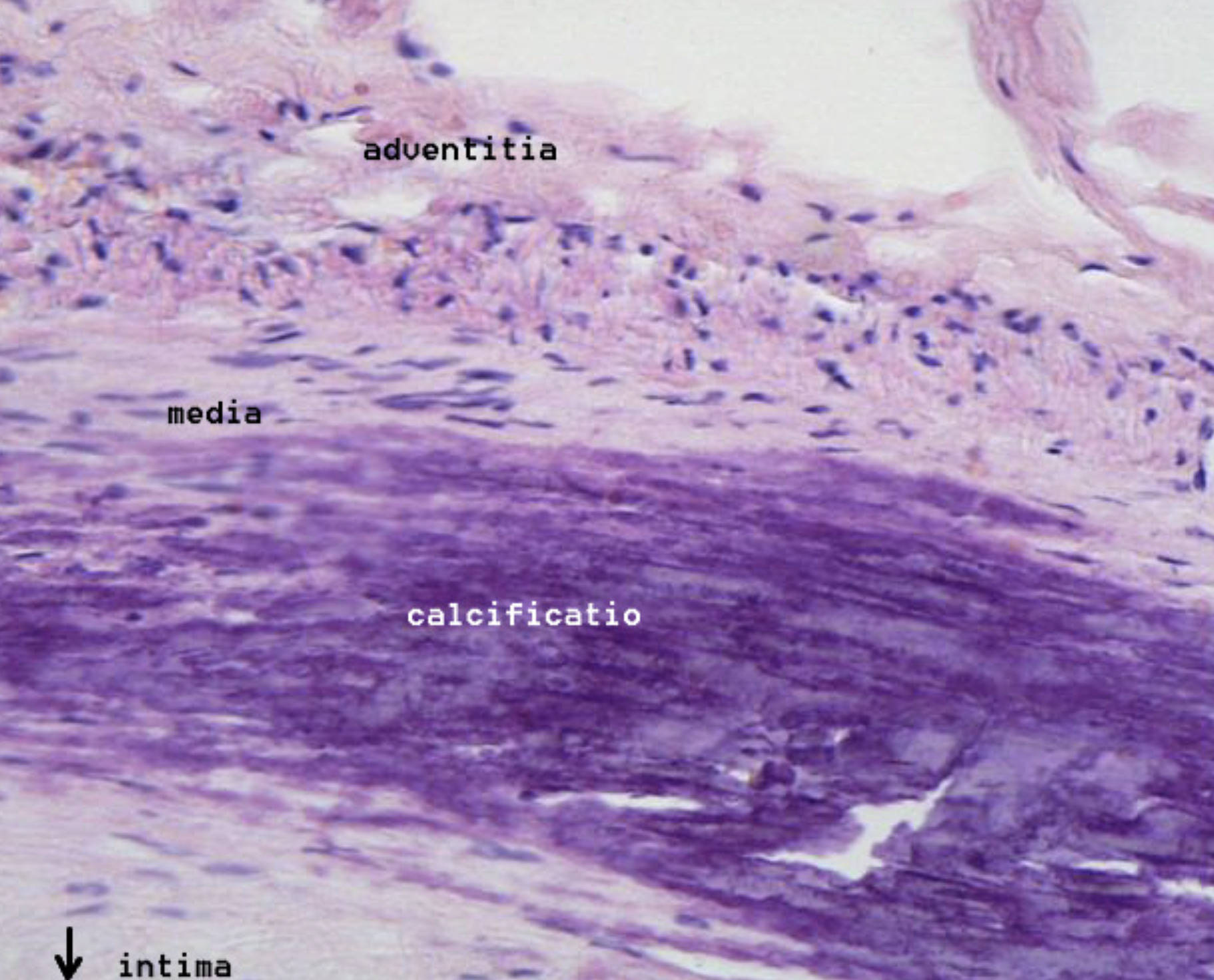
adventitia: This is the outermost layer of the arterial wall, composed primarily of connective tissue. It provides structural support and anchors the artery to surrounding tissues, containing nerves and blood vessels that supply the arterial wall itself.
media: The middle layer of the artery, comprised mainly of smooth muscle cells and elastic fibers. This layer is responsible for regulating arterial diameter and blood pressure through contraction and relaxation.
calcificatio: This prominently stained purple area indicates significant calcium deposition within the arterial wall, a hallmark of advanced atherosclerosis. This calcification contributes to arterial stiffness and is a major factor in the progression of cardiovascular disease.
intima: The innermost layer of the artery, directly exposed to the blood flow. In healthy arteries, it is a thin layer of endothelial cells; however, in atherosclerosis, it thickens significantly due to plaque formation, as indicated by the arrow pointing to the affected region.
Calcific atherosclerosis is a severe manifestation of arterial disease characterized by the deposition of calcium salts within the arterial walls, particularly within atherosclerotic plaques. This process, often referred to as “hardening of the arteries,” significantly contributes to arterial stiffness and dysfunction. The image provides a high-magnification view, clearly showcasing this pathological calcification alongside the distinct layers of the arterial wall.
The presence of calcification indicates a more advanced and complex stage of atherosclerosis. While atherosclerosis primarily involves the accumulation of lipids, inflammatory cells, and fibrous tissue, the subsequent calcification exacerbates the mechanical properties of the artery. This leads to:
- Increased arterial rigidity
- Reduced elasticity
- Compromised blood flow regulation
- Increased risk of plaque rupture
These factors collectively contribute to a higher risk of adverse cardiovascular events. The microscopic appearance of dense, amorphous purple deposits within the plaque highlights the extent of mineral deposition.
The Pathophysiology of Arterial Calcification
Arterial calcification is not merely a passive process but an active, regulated mechanism involving cellular and molecular pathways similar to bone formation. It typically occurs in two main forms: intimal calcification, which is associated with atherosclerotic plaques, and medial calcification (Mönckeberg’s arteriosclerosis), which affects the middle layer of the artery and is often seen in conditions like diabetes and chronic kidney disease. The image primarily depicts intimal calcification, evident within the thickened intima layer.
The process begins with the differentiation of vascular smooth muscle cells (VSMCs) within the arterial wall into osteoblast-like cells. These transformed cells then initiate the deposition of calcium and phosphate, forming hydroxyapatite crystals, which are the main mineral component of bone. Various factors, including inflammation, oxidative stress, dyslipidemia, and imbalances in calcium and phosphate metabolism, drive this cellular transformation and mineral deposition. The prominent purple staining for “calcificatio” in the micrograph dramatically illustrates the advanced stage of this mineral accumulation within the arterial plaque. This extensive calcium deposit stiffens the artery, making it less compliant and increasing pulse wave velocity, which in turn elevates systolic blood pressure and places greater strain on the heart.
Furthermore, calcification within atherosclerotic plaques can influence plaque stability. While initially thought to stabilize plaques, growing evidence suggests that microcalcifications (small, scattered calcium deposits) can actually increase plaque vulnerability to rupture. Larger, confluent calcifications, as seen in the image, tend to be associated with more stable plaques, but they still contribute to arterial stiffness and can impede effective revascularization procedures. The interplay between the adventitia, media, and intima, normally responsible for arterial health, becomes profoundly disrupted by this calcification. The media, which should allow for arterial flexibility, is indirectly affected by the stiffening caused by the intimal calcification, impairing the artery’s overall ability to respond to hemodynamic forces.
Clinical Implications and Management
The presence of arterial calcification is a strong independent predictor of cardiovascular events, including myocardial infarction, stroke, and peripheral artery disease. Its detection often indicates advanced atherosclerotic burden. Clinically, arterial calcification can be identified through imaging techniques such as computed tomography (CT) scans, which can quantify coronary artery calcium scores. These scores are valuable tools for risk stratification in asymptomatic individuals.
Management of calcific atherosclerosis focuses on aggressive control of traditional cardiovascular risk factors. This includes pharmacological therapies such as statins to lower cholesterol, antiplatelet agents to prevent thrombosis, and antihypertensive medications to manage blood pressure. Lifestyle modifications, including a healthy diet, regular exercise, and smoking cessation, are also critical. While there are currently no treatments to reverse established arterial calcification, ongoing research explores novel therapeutic strategies aimed at inhibiting its progression.
Understanding the microscopic pathology of calcific atherosclerosis, as vividly presented in this image, is fundamental for both diagnosis and the development of more effective treatment and prevention strategies. The visible calcium deposits underscore the severity and chronicity of this disease.

