The baroreceptor reflex is a critical mechanism that helps regulate blood pressure by detecting changes and initiating responses to restore balance. This diagram showcases how increased or decreased blood pressure triggers baroreceptor firing, influencing cardiac output and vascular tone to achieve homeostasis, ensuring the circulatory system functions optimally.
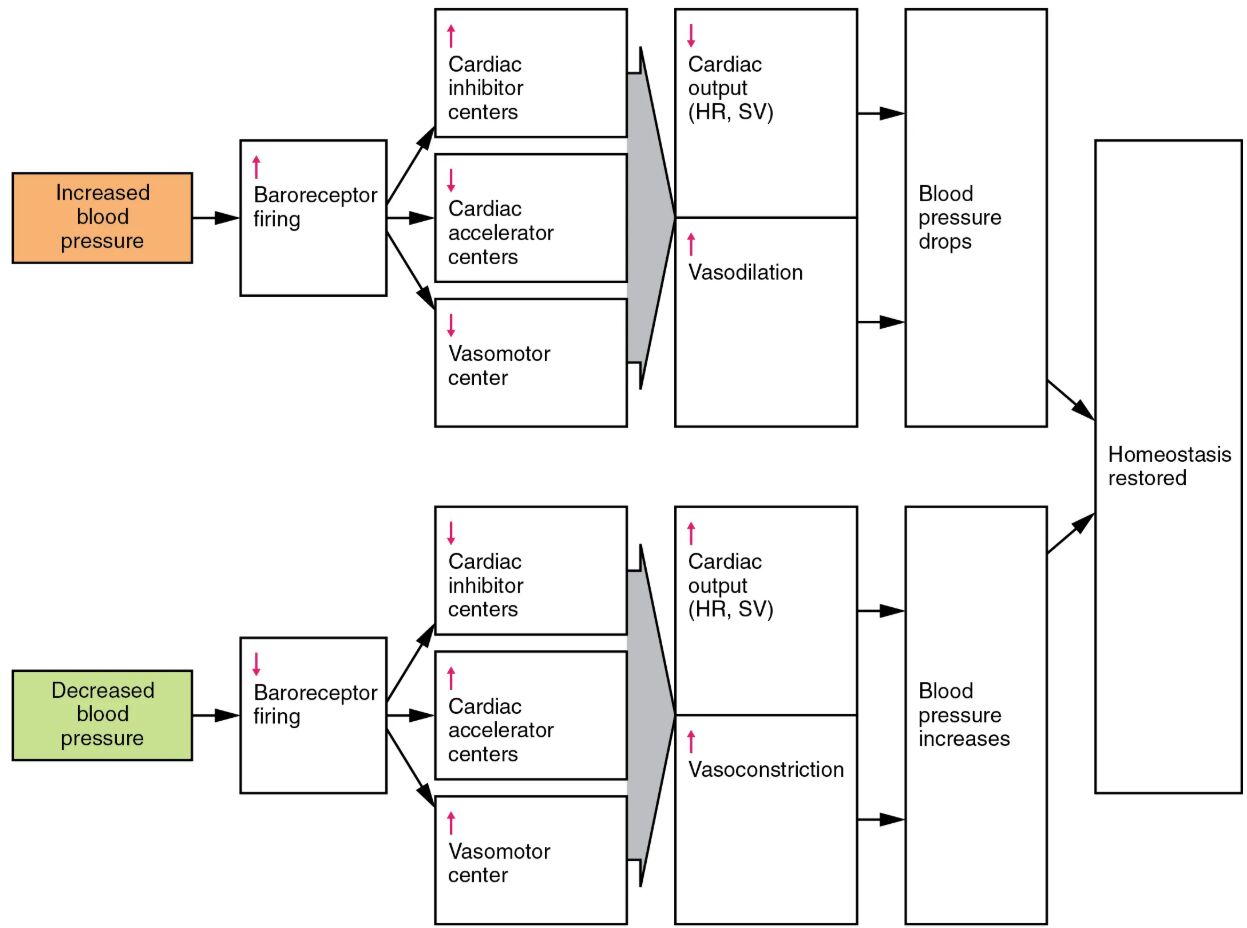
Increased blood pressure When blood pressure rises, this condition signals the body to adjust circulation to prevent strain on vessels. It prompts an increase in baroreceptor firing to initiate corrective mechanisms.
Baroreceptor firing This process involves sensory nerves detecting pressure changes in the arterial walls. Increased firing rates signal the brain to reduce cardiac activity and dilate vessels to lower pressure.
Cardiac inhibitor centers These centers in the medulla oblongata slow heart rate and reduce contractility. They help decrease cardiac output to counteract elevated blood pressure.
Cardiac accelerator centers Typically active to increase heart rate, these centers are inhibited during high pressure scenarios. Their suppression aids in reducing overall cardiac output.
Vasomotor center This region controls vascular tone and promotes vasodilation during high pressure. It adjusts blood vessel diameter to decrease peripheral resistance.
Vasodilation Widening of blood vessels reduces pressure by increasing blood flow capacity. This response lowers blood pressure back toward normal levels.
Cardiac output (HR, SV) Heart rate (HR) and stroke volume (SV) are reduced to decrease the amount of blood pumped. This adjustment helps stabilize systemic pressure.
Blood pressure drops As a result of these combined efforts, blood pressure decreases to a safer range. This drop signals the end of the acute response phase.
Decreased blood pressure A drop in blood pressure triggers a compensatory mechanism to prevent inadequate perfusion. It leads to reduced baroreceptor firing, prompting an increase in cardiac activity.
Homeostasis restored Through these adjustments, the body returns to a balanced state, ensuring consistent blood pressure. This restoration supports vital organ function and overall health.
The Role of Baroreceptors in Blood Pressure Regulation
Baroreceptor firing is the cornerstone of rapid blood pressure adjustments. These sensors, located in the carotid sinus and aortic arch, respond dynamically to stretch caused by pressure changes.
- Increased pressure stretches baroreceptors, boosting firing rates to signal the brain.
- Decreased pressure reduces stretch, lowering firing rates to trigger a compensatory rise.
- The reflex operates within milliseconds, providing immediate feedback to the cardiovascular system.
- Baroreceptors adapt over time to sustained pressure changes, maintaining long-term stability.
- This sensitivity is crucial for preventing both hypertension and hypotension.
How Cardiac Centers Influence Circulation
Cardiac inhibitor centers and cardiac accelerator centers work in tandem to modulate heart function. Their activation or inhibition directly impacts cardiac output.
- Inhibitor centers release parasympathetic signals to slow heart rate during high pressure.
- Accelerator centers increase sympathetic activity to raise heart rate when pressure drops.
- Stroke volume adjusts through changes in venous return and contractility.
- These centers integrate with the autonomic nervous system for precise control.
- Hormonal inputs, like adrenaline, can amplify their effects during stress.
The Impact of Vasomotor Control
The vasomotor center plays a pivotal role in adjusting vascular tone to regulate blood pressure. Its influence on vasodilation and vasoconstriction is essential for homeostasis.
- During high pressure, the center promotes vasodilation to reduce peripheral resistance.
- In low pressure scenarios, it triggers vasoconstriction to elevate pressure.
- Smooth muscle contraction in arterioles is the primary target of these adjustments.
- Endothelial factors, such as nitric oxide, enhance vasodilation responses.
- This dual action ensures blood distribution aligns with tissue needs.
Mechanisms of Vasodilation and Vasoconstriction
Vasodilation and vasoconstriction are opposing processes that fine-tune blood flow. They respond to baroreceptor signals to stabilize blood pressure.
- Vasodilation widens vessel lumens, reducing pressure by decreasing resistance.
- Vasoconstriction narrows vessels, increasing pressure to enhance perfusion.
- These changes affect capillary beds, influencing oxygen delivery and waste removal.
- Sympathetic nervous system activation drives vasoconstriction during hypotension.
- The balance prevents overcompensation, maintaining circulatory equilibrium.
Achieving Homeostasis Through Reflexes
The ultimate goal of these reflexes is to restore homeostasis by normalizing blood pressure. This process involves a coordinated response across multiple systems.
- Blood pressure drops after vasodilation and reduced cardiac output in hypertension.
- Increased pressure follows vasoconstriction and elevated cardiac output in hypotension.
- The feedback loop resets baroreceptor firing once balance is achieved.
- Chronic dysregulation can lead to conditions like heart failure or shock.
- Understanding these mechanisms aids in developing effective treatments.
The baroreceptor reflex exemplifies the body’s remarkable ability to maintain blood pressure and homeostasis under varying conditions. By integrating sensory input, cardiac regulation, and vascular adjustments, this system ensures consistent perfusion, offering valuable insights into cardiovascular health.

