The heart’s ability to adapt to varying physiological demands relies heavily on its autonomic innervation, a sophisticated system governed by the brain. This process involves the cardioaccelerator and cardioinhibitory centers in the medulla oblongata, which regulate heart rate and force through sympathetic and parasympathetic pathways. Exploring this intricate network provides a deeper understanding of cardiovascular control, offering insights into how the body maintains optimal circulation under diverse conditions.
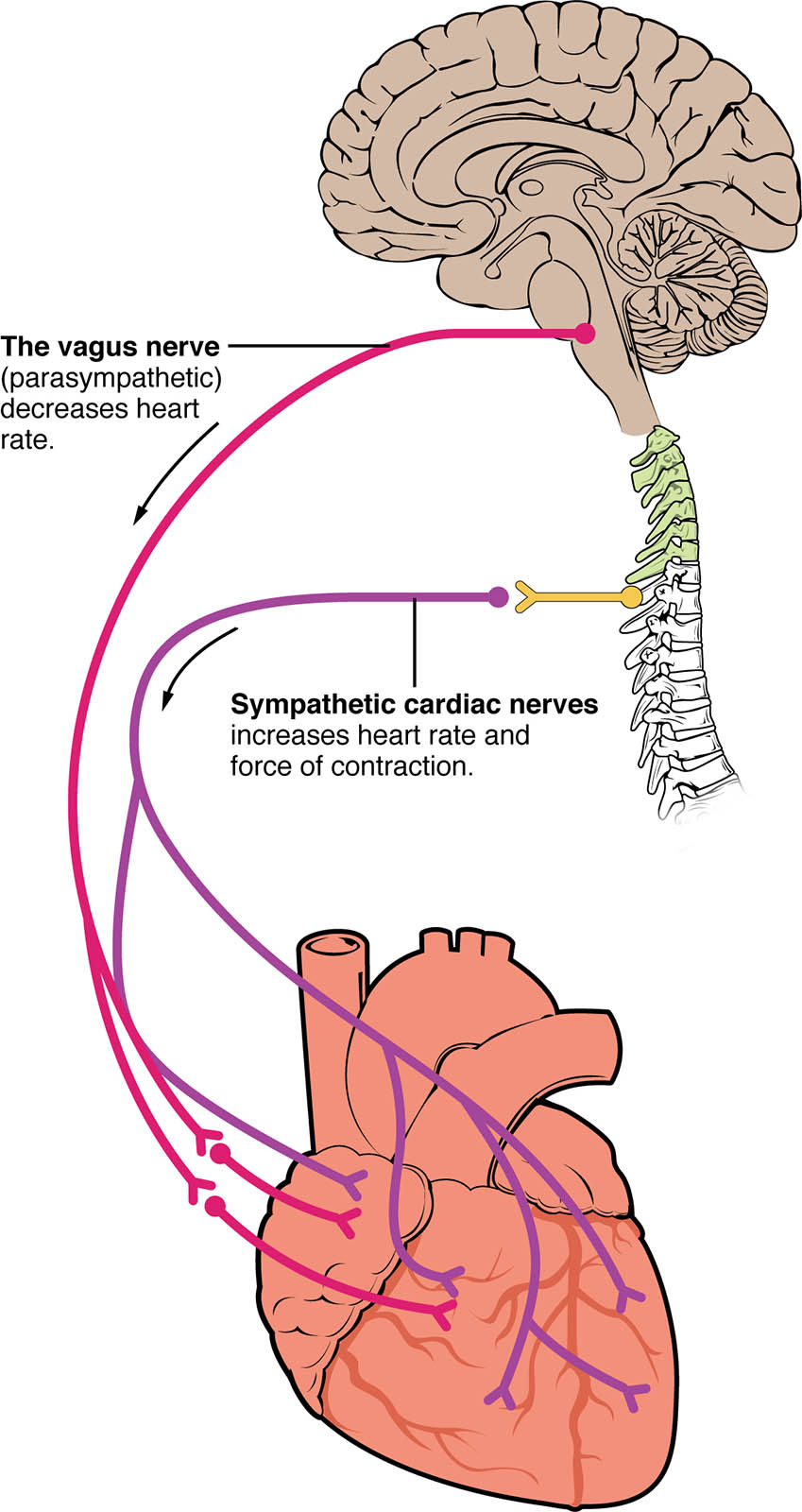
The Vagus Nerve (Parasympathetic) The vagus nerve (parasympathetic) originates from the medulla oblongata and slows heart rate by releasing acetylcholine at the sinoatrial node. This nerve plays a crucial role in maintaining a balanced heart rhythm during rest, counteracting excitatory signals when needed.
Sympathetic Cardiac Nerves Sympathetic cardiac nerves arise from the thoracic spinal cord and increase both heart rate and force of contraction through norepinephrine release. These nerves activate during stress or exercise, enhancing cardiac output to meet heightened metabolic demands.
Overview of Autonomic Control
The autonomic nervous system finely tunes heart function, ensuring adaptability to changing needs. It operates through two opposing branches that maintain cardiovascular homeostasis.
- The autonomic innervation integrates signals from the brain to the heart via neural pathways.
- The medulla oblongata houses control centers that respond to blood pressure and oxygen levels.
- Sympathetic activation accelerates heart rate, preparing the body for action.
- Parasympathetic input, via the vagus nerve (parasympathetic), promotes relaxation and recovery.
- Hormones like adrenaline amplify these neural effects during emergencies.
The Role of the Vagus Nerve
The vagus nerve (parasympathetic) serves as a key regulator of heart rate, promoting a calm state. Its influence is essential for preventing overexertion and maintaining long-term heart health.
- This nerve releases acetylcholine, slowing the sinoatrial node’s firing rate.
- It dominates during rest, reducing energy expenditure by the heart.
- Baroreceptors in the aorta trigger vagus nerve (parasympathetic) activity to lower heart rate when pressure rises.
- Damage to this nerve can lead to tachycardia, highlighting its protective role.
- Its effects are counterbalanced by sympathetic input for dynamic adjustment.
Parasympathetic Impact on Cardiac Function
Parasympathetic control through the vagus nerve (parasympathetic) supports efficient heart operation. This branch ensures the heart does not overwork during low-demand periods.
- Acetylcholine binds to muscarinic receptors, decreasing pacemaker cell excitability.
- This reduces the force of atrial contraction while preserving ventricular function.
- The vagus nerve (parasympathetic) helps regulate heart rate variability, a marker of health.
- Chronic stress can diminish its effectiveness, leading to irregular rhythms.
- Meditation or deep breathing enhances its calming influence.
Sympathetic Cardiac Nerves in Action
Sympathetic cardiac nerves drive the heart’s response to stress, boosting performance when needed. They ensure the body can cope with physical or emotional challenges.
- Norepinephrine increases the rate of depolarization in the sinoatrial node.
- These nerves enhance contractility, improving stroke volume during exercise.
- Sympathetic cardiac nerves are activated by the fight-or-flight response.
- Overactivation can contribute to hypertension if not balanced by parasympathetic input.
- Thyroid hormones T3 and T4 can amplify their effects on heart rate.
Sympathetic Effects on Heart Dynamics
The influence of sympathetic cardiac nerves extends beyond rate to overall cardiac strength. This system prepares the heart for increased workload efficiently.
- Beta-adrenergic receptors mediate the increase in contractility and rate.
- Enhanced calcium influx strengthens myocardial contraction.
- Sympathetic cardiac nerves support the heart during acute stress or injury.
- Prolonged activation may lead to cardiac hypertrophy in some cases.
- Exercise training can optimize their responsiveness for better endurance.
Integration with Hormonal Systems
The autonomic system works alongside hormonal signals to regulate heart function. This synergy ensures a comprehensive approach to cardiovascular control.
- Adrenaline from the adrenal glands reinforces sympathetic cardiac nerves activity.
- Cortisol modulates the sensitivity of cardiac tissues to neural input.
- The vagus nerve (parasympathetic) counters hormonal surges during recovery.
- Thyroid hormones influence baseline heart rate, affecting autonomic balance.
- Electrolyte levels, like potassium, fine-tune neural signaling to the heart.
Clinical Relevance of Autonomic Innervation
Understanding autonomic innervation aids in diagnosing and managing heart conditions. This knowledge is vital for tailoring effective treatments.
- Imbalances can lead to arrhythmias, requiring medical intervention.
- Sympathetic cardiac nerves overactivity is linked to heart failure progression.
- Vagal stimulation is explored as a therapy for atrial fibrillation.
- Monitoring heart rate variability assesses autonomic innervation health.
- Drugs like beta-blockers target these pathways to restore balance.
In conclusion, the autonomic innervation of the heart, driven by the vagus nerve (parasympathetic) and sympathetic cardiac nerves, exemplifies the body’s remarkable ability to adapt. This dual control system ensures the heart responds appropriately to rest, exercise, and stress, maintaining vital circulation. Delving into these mechanisms fosters a greater appreciation of cardiovascular physiology and supports efforts to enhance heart health.

