Atherosclerosis is a progressive condition where plaques formed by fatty and calcified deposits build up within artery walls, potentially leading to serious cardiovascular issues. This image combines a diagram illustrating plaque formation and a micrograph of a coronary artery showing connective tissue buildup, offering a dual perspective on this disease at ×40 magnification. Examining these visuals provides valuable insights into the structural changes and health implications of atherosclerosis in the cardiovascular system.
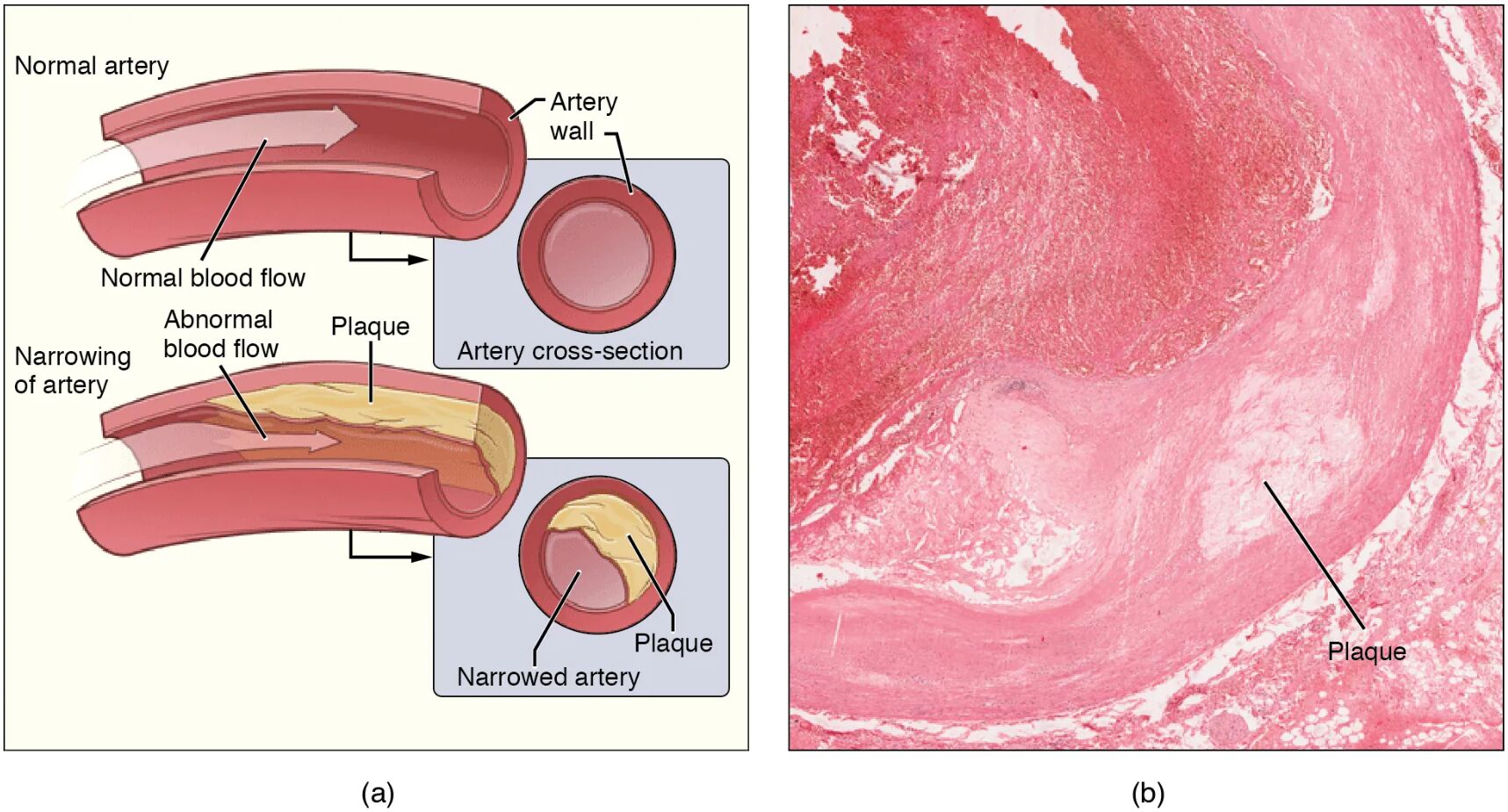
Artery wall: The artery wall is the layered structure of an artery, including the intima, media, and adventitia, which normally maintains elasticity and blood flow. In atherosclerosis, this wall thickens due to plaque accumulation, reducing its flexibility and narrowing the lumen.
Plaque: Plaque consists of fatty deposits, cholesterol, calcium, and cellular debris that accumulate within the artery wall, forming a hard, irregular mass. This buildup obstructs blood flow and can lead to complications like thrombosis or artery blockage.
Connective tissue: Connective tissue within the artery wall, as seen in the micrograph, provides structural support but becomes excessive in atherosclerosis, contributing to plaque stability. Its overgrowth can stiffen the artery, further impairing blood flow and increasing the risk of rupture.
Lumen: The lumen is the inner open space of the artery through which blood flows, normally wide and unobstructed. In atherosclerosis, the lumen narrows due to plaque and connective tissue buildup, limiting oxygen delivery to tissues.
Anatomical Structure of Atherosclerosis
The artery’s internal anatomy undergoes significant changes in atherosclerosis, and this diagram and micrograph provide a clear view of these alterations. Understanding the affected components helps in recognizing the disease’s progression.
- The artery wall thickens as plaque develops, altering its normal layered structure.
- The plaque forms a barrier within the artery wall, disrupting smooth blood flow.
- The connective tissue’s increased presence stabilizes the plaque but adds rigidity.
- The lumen’s reduction reflects the cumulative impact of these changes.
This process often begins with endothelial injury, setting the stage for plaque growth.
Physiological Impact and Symptoms
Atherosclerosis affects blood flow and oxygen delivery, leading to a range of physiological effects. The images illustrate how these changes manifest in the coronary artery.
- The artery wall’s thickening increases resistance, raising blood pressure upstream.
- The plaque’s presence can trigger clot formation, risking heart attack or stroke.
- The connective tissue’s buildup contributes to arterial stiffness, reducing elasticity.
- The lumen’s narrowing may cause chest pain or shortness of breath, signaling ischemia.
Symptoms depend on the artery affected, with coronary involvement being particularly critical.
Causes and Risk Factors
The development of atherosclerosis involves multiple factors that contribute to plaque formation. Identifying these aids in prevention and early intervention.
- High cholesterol levels promote plaque accumulation within the artery wall.
- Hypertension damages the endothelium, initiating atherosclerosis progression.
- Smoking and diabetes accelerate connective tissue and plaque buildup.
- Genetic predisposition increases susceptibility, often linked to family history.
Lifestyle modifications, like a heart-healthy diet, can mitigate these risks.
Diagnosis and Treatment Options
Diagnosing and managing atherosclerosis requires a tailored approach based on its severity. Imaging and clinical assessments guide treatment decisions.
- Angiography visualizes the lumen to assess plaque extent and severity.
- Statins lower cholesterol, reducing plaque growth in the artery wall.
- Angioplasty or stenting opens the lumen, relieving obstruction caused by plaque.
- Surgical bypass may be needed for severe connective tissue and plaque buildup.
Regular monitoring with stress tests tracks disease progression.
Clinical Relevance and Long-Term Outlook
Understanding the implications of atherosclerosis is essential for long-term health management. The condition’s impact varies with the extent of arterial involvement.
- The artery wall’s health determines flexibility, affecting overall circulation.
- The plaque’s stability influences rupture risk, a key factor in acute events.
- The connective tissue’s role can complicate surgical interventions if excessive.
- The lumen’s patency post-treatment predicts quality of life and survival rates.
Lifestyle changes and medications improve outcomes significantly.
Conclusion
This diagram and micrograph of atherosclerosis provide a detailed view of the artery wall, plaque, connective tissue, and lumen, illustrating the disease’s impact on coronary arteries. By showcasing the buildup of fatty deposits and connective tissue, it highlights the importance of early detection and management to prevent complications like heart attack or stroke. This understanding equips individuals with the knowledge to address atherosclerosis effectively, promoting better cardiovascular health.

