Discover the life-saving technology of artificial heart valves, essential medical devices designed to replace diseased or damaged native heart valves. These prosthetics restore proper blood flow through the heart, significantly improving cardiac function and enhancing the quality of life for countless patients globally.
Understanding the Artificial Heart Valve Diagram
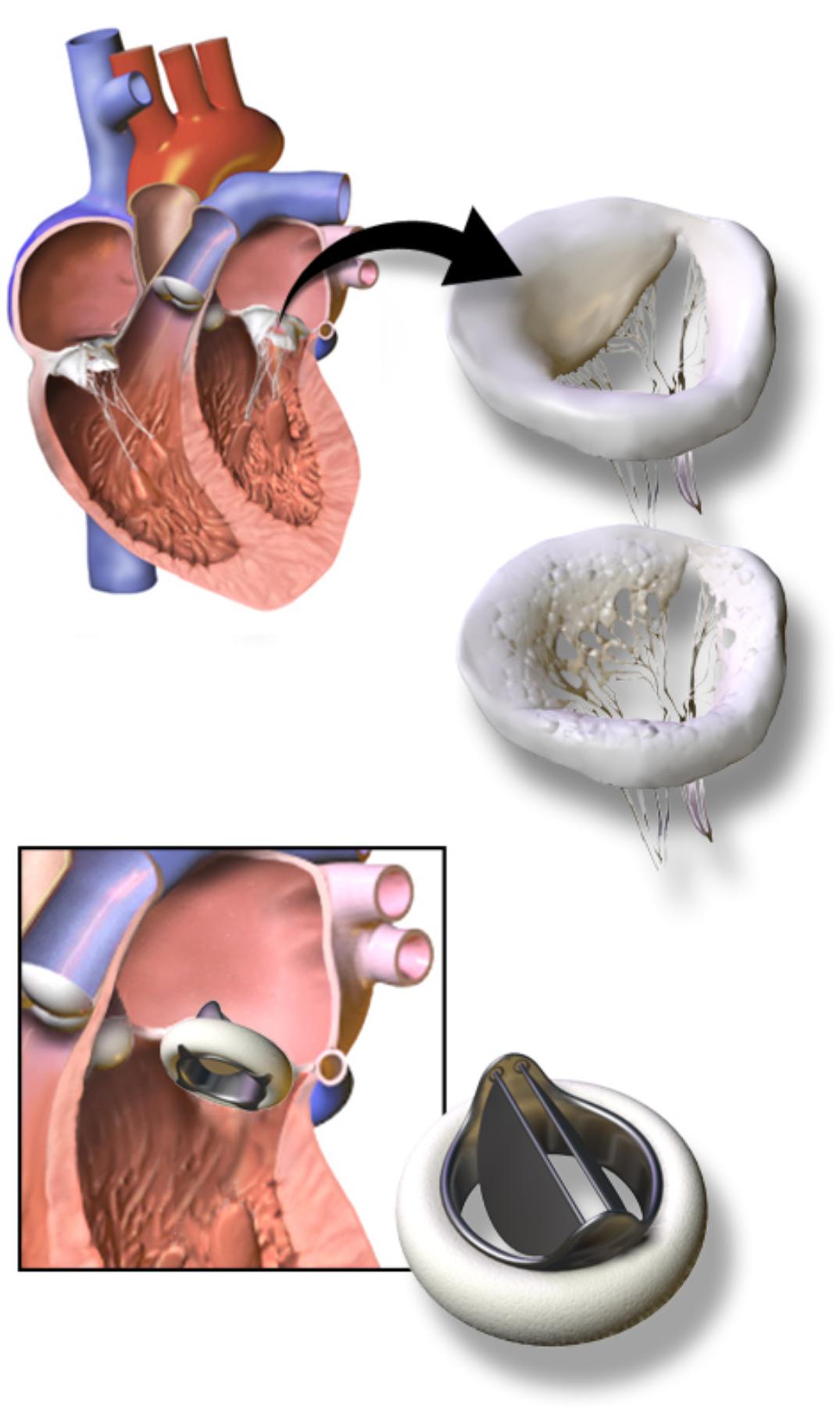
Heart (cutaway view): This illustrates a section of the human heart, showing its four chambers and major blood vessels. It provides anatomical context, demonstrating where the heart valves are naturally located and where an artificial valve would be implanted.
Diseased/Damaged Native Valve: This image depicts a natural heart valve that has become compromised, likely due to conditions such as stenosis (narrowing) or regurgitation (leaking). Its impaired structure indicates a failure to properly open or close, thereby disrupting efficient blood flow.
Artificial Heart Valve (top right): This illustrates a mechanical prosthetic heart valve, typically constructed from durable materials such as pyrolytic carbon and metal. These valves are designed for longevity and offer excellent hemodynamic performance, ensuring unidirectional blood flow.
Artificial Heart Valve (bottom right, implanted): This image shows the artificial heart valve once it has been surgically implanted into the heart. It highlights how the prosthetic device integrates within the cardiac structure to replace the function of a damaged native valve, restoring efficient blood circulation.
The Critical Role of Heart Valves
The human heart, a remarkable muscular pump, relies on four perfectly synchronized valves to ensure the unidirectional flow of blood through its chambers and into the circulatory system. These valves—the tricuspid, pulmonary, mitral, and aortic valves—open and close with each heartbeat, preventing backflow and maintaining efficient blood circulation. When one or more of these native valves become diseased or damaged, the heart’s ability to pump blood effectively is severely compromised, leading to a range of symptoms and potentially life-threatening conditions.
Valve dysfunction can manifest in two primary ways: stenosis or regurgitation. Stenosis refers to the narrowing of a valve opening, which restricts blood flow and forces the heart to work harder to push blood through the constricted opening. This increased workload can lead to heart muscle thickening (hypertrophy) and eventual heart failure. Conversely, regurgitation (or insufficiency) occurs when a valve does not close completely, allowing blood to leak backward into the preceding chamber. This inefficiency also increases the heart’s workload, as it must pump the same blood multiple times, leading to chamber dilation and reduced cardiac output.
Historically, severe valve disease carried a grim prognosis, often leading to progressive heart failure and early mortality. However, advancements in cardiovascular surgery and biomaterials have revolutionized treatment options, with the development of artificial heart valves being a monumental leap forward. These prosthetic devices are engineered to mimic the function of healthy native valves, meticulously controlling blood flow and alleviating the strain on the heart. The choice of valve type, surgical approach, and long-term management are critical considerations in restoring patient health and ensuring durability.
- Heart valves ensure unidirectional blood flow.
- Dysfunction includes stenosis (narrowing) and regurgitation (leaking).
- Artificial valves replace diseased native valves.
- They significantly improve cardiac function.
Types of Artificial Heart Valves
Artificial heart valves generally fall into two main categories: mechanical valves and bioprosthetic (tissue) valves. Each type presents distinct advantages and disadvantages, influencing the decision-making process between patient and surgeon.
Mechanical Heart Valves: These valves are constructed from durable synthetic materials, most commonly pyrolytic carbon, a material known for its strength and biocompatibility. They typically feature a rigid ring with one or two tilting discs that open and close to regulate blood flow. The primary advantage of mechanical valves is their exceptional durability, often lasting 20-30 years or even longer. This longevity makes them particularly suitable for younger patients, as it minimizes the need for reoperation. However, a significant drawback is their thrombogenicity; mechanical valves present a surface where blood clots can easily form. Consequently, patients with mechanical valves require lifelong anticoagulation therapy (blood thinners like warfarin) to prevent clot formation, which carries its own risks, including bleeding complications.
Bioprosthetic Heart Valves: Also known as tissue valves, these are derived from animal tissue, typically porcine (pig) or bovine (cow) pericardium, which is treated to reduce antigenicity and prevent calcification. Some are also made from human donor valves (allografts). Bioprosthetic valves are designed to closely mimic the natural structure and function of native heart valves. Their main advantage is their lower thrombogenicity compared to mechanical valves, meaning patients often do not require lifelong anticoagulation, or at least a less intensive regimen. This makes them a preferred choice for older patients, women of childbearing potential, or individuals with a high risk of bleeding. The primary limitation of bioprosthetic valves is their limited durability; they tend to degenerate over time due to calcification and structural fatigue, often requiring reoperation within 10-15 years.
Surgical Implantation and Post-Operative Care
The implantation of an artificial heart valve is a major cardiac surgical procedure, typically performed under general anesthesia with the patient on cardiopulmonary bypass (a heart-lung machine). The surgeon carefully excises the damaged native valve and then sutures the prosthetic valve into its place. The exact surgical approach depends on the affected valve and the patient’s overall health, but common techniques include open-heart surgery via a sternotomy or minimally invasive approaches.
Post-operative care is critical for the success and longevity of an artificial valve. This includes meticulous wound care, pain management, and a gradual return to activity. Patients with mechanical valves will begin lifelong anticoagulation therapy, requiring regular monitoring of their international normalized ratio (INR) to ensure the blood is thinned sufficiently to prevent clots but not excessively to cause bleeding. All patients with artificial valves are also at an increased risk of infective endocarditis (an infection of the heart lining or valves) and typically receive prophylactic antibiotics before dental procedures or other interventions that might introduce bacteria into the bloodstream. Regular follow-up with a cardiologist, including echocardiograms, is essential to monitor valve function and detect any potential complications early.
Conclusion
Artificial heart valves represent a pinnacle of medical engineering, offering a transformative solution for patients suffering from severe valvular heart disease. By meticulously restoring the heart’s ability to pump blood efficiently, these devices alleviate symptoms, improve cardiac function, and significantly enhance the quality of life for countless individuals. While the choice between mechanical and bioprosthetic valves involves careful consideration of durability, the need for anticoagulation, and patient-specific factors, both options stand as powerful testaments to the continuous innovation in cardiovascular medicine, offering renewed hope and health to those with compromised hearts.

