This diagram provides a comprehensive overview of aortic coarctation and its repair using various advanced imaging techniques. Aortic coarctation is a congenital narrowing of the aorta, often located near the ductus arteriosus, which significantly impedes blood flow to the lower body. The diverse images—A: ‘Black-blood’ oblique sagittal view, B: 3D contrast-enhanced CT angiogram, C: 3D contrast-enhanced MR angiogram, and D: another 3D contrast-enhanced MR angiogram—collectively demonstrate the condition’s characteristics and potential post-surgical complications. Understanding these visual details is crucial for accurate diagnosis, treatment planning, and long-term management of this complex cardiovascular anomaly.
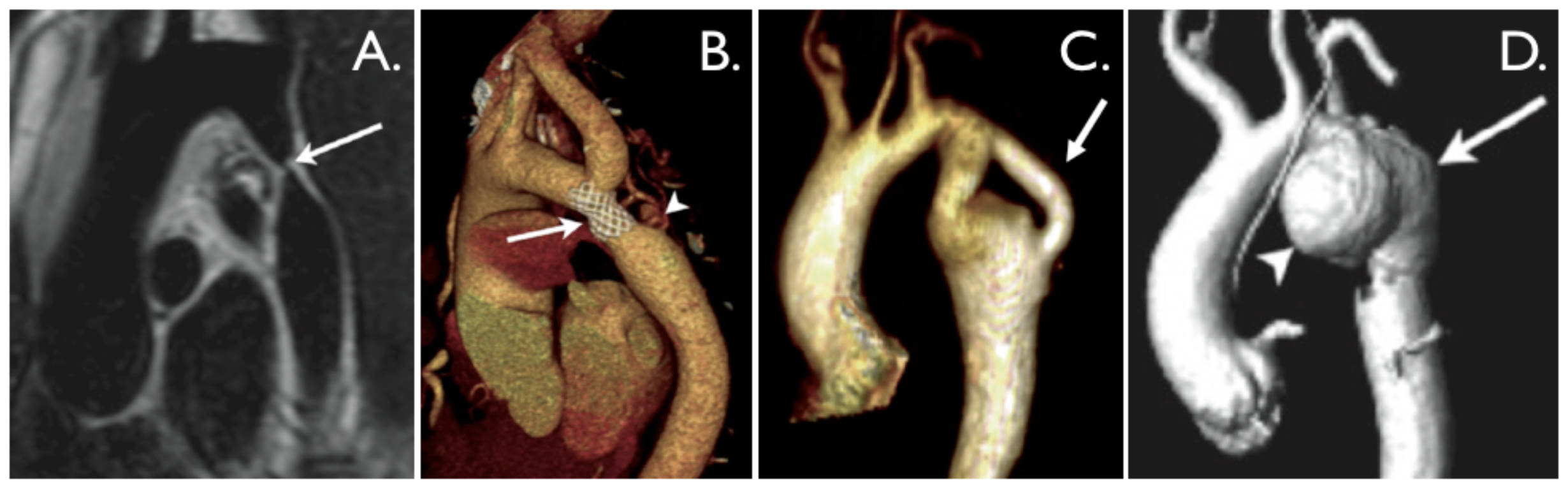
A. Arrow: This arrow clearly indicates a discrete and tight coarctation at the aortic isthmus, which is the narrowed segment of the aorta. This severe constriction significantly obstructs normal blood flow from the heart to the rest of the body, particularly to the lower extremities, increasing the workload on the heart. Such a tight narrowing necessitates intervention to restore adequate circulation.
B. Arrow: The arrow in this 3D CT angiogram highlights a mildly narrowed bare metal stent, which has been placed to open the coarctation. Despite the stent, some residual narrowing is evident, suggesting the possibility of re-coarctation or incomplete expansion. This stent partially overlies the origin of the left subclavian artery, a critical consideration for blood flow to the left arm and brain.
B. Arrowhead: The arrowhead points to a subtle pseudo-aneurysm located at the distal end of the stent. A pseudo-aneurysm is a contained rupture of the arterial wall, where blood leaks out but is confined by surrounding tissues, creating a pulsatile hematoma. Its presence suggests a potential complication from the stenting procedure, requiring close monitoring.
C. Arrow: This arrow indicates a ‘jump’ bypass graft positioned posteriorly, used to circumvent areas of aortic arch hypoplasia and coarctation. This surgical bypass diverts blood flow around the narrowed or underdeveloped segments of the aorta, improving systemic circulation. Such grafts are often employed in complex cases where direct repair is not feasible.
D. Arrowhead: The arrowhead highlights a large pseudo-aneurysm that has developed after a previous patch angioplasty repair. This significant bulge represents a serious complication, indicating a weakness in the aortic wall at the site of the prior repair. The potential for rupture makes its identification critical for patient management.
D. Arrow: The arrow points to the true lumen of the aorta, visible posteriorly to the pseudo-aneurysm. The true lumen is the actual, patent channel through which blood flows, distinguishing it from the false lumen created by the pseudo-aneurysm. Visualizing both structures helps in understanding the extent of the complication and planning subsequent interventions.
Introduction to Aortic Coarctation
Aortic coarctation (CoA) is a congenital heart defect characterized by a localized narrowing of the aorta, the body’s main artery. This constriction typically occurs in the descending aorta, usually near the ductus arteriosus, a vessel that normally closes shortly after birth. This narrowing significantly increases the workload on the left ventricle of the heart, as it must pump blood with greater force to overcome the obstruction and ensure adequate perfusion to the lower body. Consequently, patients with uncorrected coarctation often develop hypertension in the upper extremities and experience reduced blood pressure in the lower extremities.
The clinical presentation of aortic coarctation varies widely depending on the severity of the narrowing. In severe cases, symptoms can appear shortly after birth, leading to heart failure or shock. Milder forms might go undetected until childhood or even adulthood, presenting with symptoms such as high blood pressure, headaches, cold extremities, or leg pain during exercise (claudication). The advent of advanced imaging techniques, as illustrated in this diagram, has revolutionized the diagnosis and management of this condition, allowing for precise localization of the narrowing and detailed assessment of its impact on the cardiovascular system.
Effective diagnosis and timely intervention are crucial to prevent long-term complications associated with untreated aortic coarctation. These complications can include left ventricular hypertrophy, aortic aneurysm or dissection, premature coronary artery disease, and stroke. Early recognition through careful clinical examination and appropriate imaging studies is therefore paramount for improving patient outcomes.
Key characteristics and associated conditions often observed with aortic coarctation include:
- Bicuspid Aortic Valve: Approximately 50-85% of patients with CoA also have a bicuspid aortic valve, a congenital heart defect where the aortic valve has two cusps instead of the normal three.
- Turner Syndrome: Females with Turner syndrome (XO karyotype) have an increased incidence of aortic coarctation and other cardiovascular anomalies.
- Collateral Circulation: The body often develops collateral blood vessels to bypass the narrowed segment, providing alternative pathways for blood flow to the lower body.
- Hypertension: Elevated blood pressure, especially in the upper extremities, is a classic sign due to increased resistance to blood flow.
- Left Ventricular Hypertrophy: The left ventricle thickens over time as it works harder to pump blood through the narrowed aorta.
These associated factors underscore the systemic impact of aortic coarctation.
The Pathophysiology and Clinical Manifestations of Coarctation
The physiological consequence of aortic coarctation is a pressure gradient across the narrowed segment of the aorta. Proximal to the coarctation, blood pressure is significantly elevated, leading to increased afterload on the left ventricle. This chronic pressure overload causes the left ventricle to undergo hypertrophy, thickening its walls to generate more force. Distal to the coarctation, blood pressure is lower, potentially leading to hypoperfusion of the abdominal organs and lower extremities. The body attempts to compensate for this reduced flow by developing an extensive network of collateral arteries, primarily involving intercostal arteries and internal mammary arteries, which bypass the coarctation to supply blood to the areas below the narrowing. While these collaterals can partially alleviate the effects of the obstruction, they are rarely sufficient to normalize blood flow and pressure.
Clinically, patients with severe coarctation often present with signs of heart failure in infancy, including poor feeding, lethargy, and respiratory distress. In older children and adults, symptoms are more subtle and may include hypertension (especially in the upper limbs), headaches, epistaxis (nosebleeds), and claudication (leg pain with exercise) due to insufficient blood flow to the lower extremities. A classic physical finding is a significant difference in blood pressure between the upper and lower limbs, with lower pressures and weaker pulses in the legs compared to the arms. A systolic murmur may also be heard over the back, reflecting turbulent flow through the narrowed aorta.
Multi-Modality Imaging in Diagnosis and Follow-Up
The diagnosis and comprehensive evaluation of aortic coarctation heavily rely on various imaging modalities, as beautifully illustrated in the provided diagram. Each technique offers unique advantages:
- Magnetic Resonance Imaging (MRI), particularly ‘black-blood’ sequences (Image A), provides excellent anatomical detail of the aorta without ionizing radiation. It can accurately delineate the severity and extent of the coarctation, assess collateral flow, and evaluate left ventricular function and hypertrophy. MR angiography (MRA) with contrast (Images C and D) further enhances visualization of the lumen and surrounding structures, crucial for surgical planning and detecting complications.
- Computed Tomography Angiography (CTA) (Image B), utilizing intravenous contrast, offers rapid, high-resolution 3D images of the aorta and its branches. It is particularly useful for assessing calcification, stent patency, and identifying pseudo-aneurysms or other vascular complications. The detailed anatomical mapping provided by CTA is invaluable for interventional procedures.
- Echocardiography (not shown but a primary tool) is typically the initial diagnostic modality, especially in neonates and infants, providing real-time assessment of cardiac structure, function, and blood flow velocities across the coarctation.
These imaging techniques are not only crucial for initial diagnosis but also for long-term follow-up after repair, monitoring for potential complications such as recoarctation, aneurysm formation, or dissection, as demonstrated in images B, C, and D. The ability to visualize these specific findings underscores the importance of a multi-modality approach in managing patients with aortic coarctation throughout their lives.
Treatment and Long-Term Management of Aortic Coarctation
The definitive treatment for aortic coarctation is typically intervention to relieve the obstruction. The choice of treatment modality depends on the patient’s age, the anatomy of the coarctation, and the presence of associated anomalies.
- Balloon Angioplasty and Stenting: This minimally invasive catheter-based procedure involves inflating a balloon at the site of the coarctation to widen the narrowed segment, often followed by the placement of a stent (as seen in Image B) to maintain patency. This is a common approach for both native coarctation and recoarctation.
- Surgical Repair: Various surgical techniques are employed, including resection with end-to-end anastomosis, subclavian flap aortoplasty, patch aortoplasty (which can lead to complications like the pseudo-aneurysm in Image D), and bypass grafting (as seen in Image C). Surgery is often preferred in neonates and young children, or in complex cases.
Regardless of the initial repair method, long-term follow-up is essential due to the lifelong risk of complications. These can include residual hypertension, recoarctation, aneurysm formation, or aortic dissection. Regular monitoring with non-invasive imaging (MRI, CT, echocardiography) is crucial to detect these issues early and allow for timely re-intervention. Comprehensive management also includes careful blood pressure control, as hypertension can persist even after successful repair, and counseling on lifestyle modifications to optimize cardiovascular health.

