Discover the AngioJet thrombectomy system, an advanced medical device used to rapidly remove blood clots from arteries and veins. This technology is critical in treating acute thrombotic events, restoring essential blood flow, and improving outcomes for patients with life-threatening conditions such as heart attacks and deep vein thrombosis.
Understanding the AngioJet Diagram
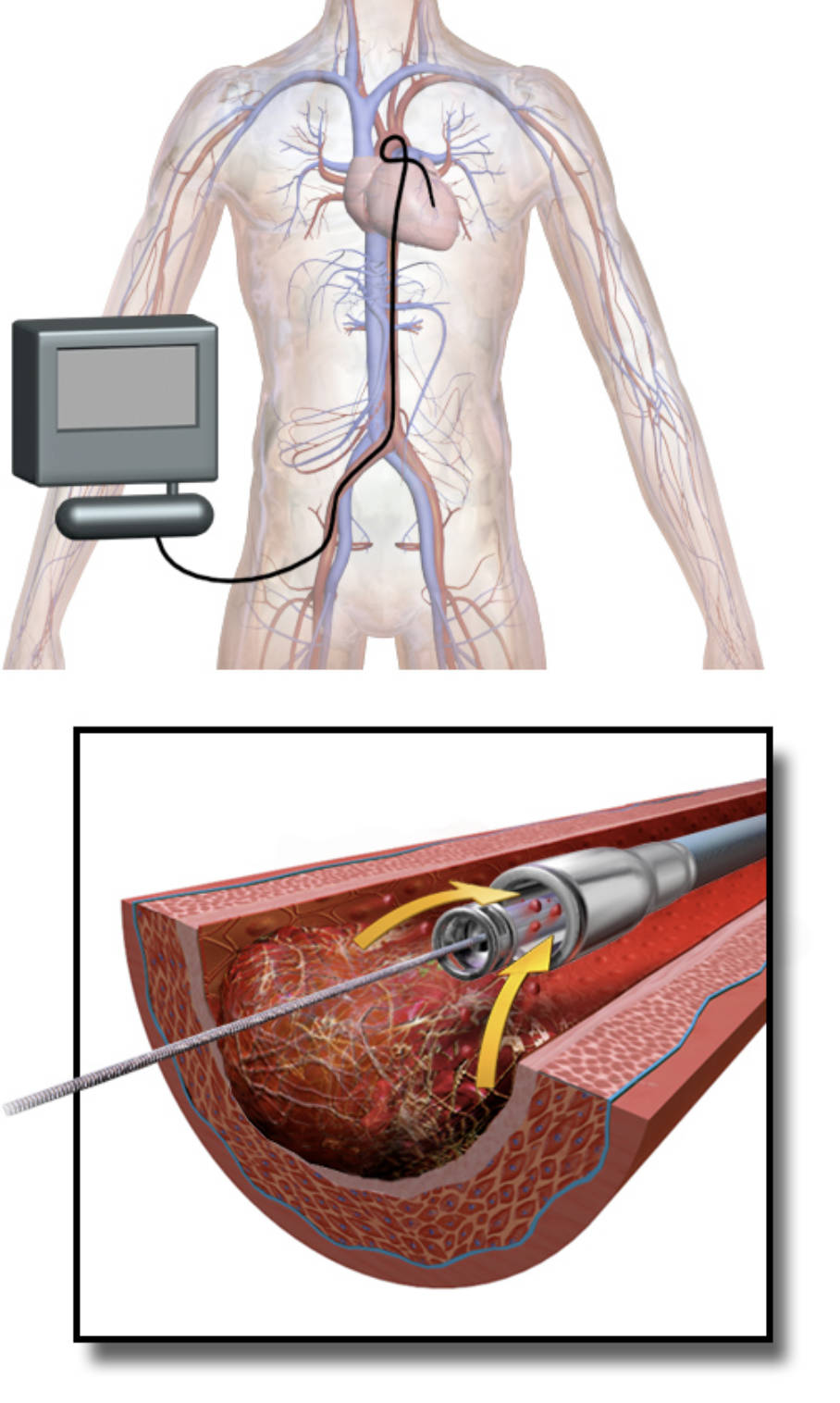
Human Anatomy (top image): This illustration depicts the human vascular system, showing how a catheter is typically inserted into a peripheral artery (often in the leg) and threaded through the arterial network towards the heart or other target vessels. It provides a visual context for the minimally invasive approach of endovascular procedures.
AngioJet Catheter in Artery (bottom image): This detailed cross-section shows the AngioJet catheter positioned within an obstructed artery, specifically targeting a blood clot (thrombus). It demonstrates the internal workings of the device, with high-velocity saline jets fragmenting the clot and a suction mechanism removing the debris.
The Challenge of Acute Thrombotic Events
Acute thrombotic events, characterized by the sudden formation of a blood clot (thrombus) within a blood vessel, represent a critical medical emergency. These clots can severely impede or completely block blood flow to vital organs, leading to conditions such as myocardial infarction (heart attack), ischemic stroke, acute limb ischemia, and deep vein thrombosis (DVT) with potential for pulmonary embolism. The rapid and effective removal of these clots is paramount to minimize tissue damage, restore organ function, and ultimately improve patient outcomes.
Traditional treatments for thrombotic events have included anticoagulant medications (blood thinners) to prevent further clot growth, and thrombolytic drugs (clot busters) which chemically dissolve the clot. While effective in many cases, thrombolytic therapy can be associated with significant risks, particularly bleeding complications, and may not be suitable for all patients. Moreover, in large or very organized clots, thrombolytics may be slow or ineffective, necessitating more direct interventional approaches.
This is where mechanical thrombectomy devices, such as the AngioJet system, play a crucial role. These devices offer a direct, physical method for extracting or aspirating thrombi, often providing a faster and more complete clot removal compared to pharmacological methods alone. The ability to rapidly re-establish blood flow is especially critical in acute settings, where every minute of ischemia (lack of blood flow) can lead to irreversible tissue damage. The AngioJet system, with its unique mechanism of action, stands out as a powerful tool in the interventional cardiologist’s and radiologist’s arsenal.
- Acute thrombotic events block blood flow.
- They can cause heart attacks, strokes, or DVT.
- Rapid clot removal is essential.
- AngioJet offers a direct mechanical thrombectomy.
The Hydrodynamic Power of AngioJet
The AngioJet thrombectomy system operates on a principle known as the Bernoulli effect, utilizing high-velocity saline jets to effectively fragment and aspirate thrombi. The device consists of a specialized catheter with multiple small, forward-facing jets located near its tip. When saline is pumped through these jets at extremely high pressure, it creates localized, high-speed fluid streams. These powerful jets are capable of physically breaking up the soft, fresh thrombus material into tiny fragments.
Crucially, the high-velocity saline jets also create a localized low-pressure zone (venturi effect) at the tip of the catheter, immediately proximal to the jets. This negative pressure generates a powerful suction force, which actively draws the fragmented clot debris and surrounding blood into aspiration lumens within the catheter. This simultaneous fragmentation and aspiration mechanism ensures that the clot material is efficiently removed from the vessel, minimizing the risk of distal embolization (where fragments travel downstream and block smaller vessels). The aspirated debris is then collected in a separate bag outside the body.
The AngioJet system’s ability to rapidly remove thrombus burden makes it particularly valuable in acute coronary syndromes (heart attacks), where immediate restoration of blood flow to the heart muscle is paramount to salvage myocardium. It is also effectively used in acute limb ischemia to prevent amputation, in pulmonary embolism to reduce right heart strain, and in deep vein thrombosis to relieve symptoms and reduce the risk of post-thrombotic syndrome. The procedural details are typically performed in a cardiac catheterization lab or interventional suite, allowing real-time visualization of the clot and catheter placement using fluoroscopy.
Clinical Applications and Patient Outcomes
The AngioJet system has diverse clinical applications across various vascular territories. In acute myocardial infarction with significant thrombus burden, its use can improve microvascular perfusion and reduce infarct size, particularly when used prior to or in conjunction with stent placement. For acute limb ischemia, rapid mechanical thrombectomy with AngioJet can quickly restore blood flow, reducing pain, preventing tissue necrosis, and potentially saving the limb from amputation. In deep vein thrombosis (DVT), especially in large veins or iliofemoral DVT, AngioJet can effectively clear the thrombus, alleviating symptoms, preventing pulmonary embolism, and reducing the long-term risk of post-thrombotic syndrome, a debilitating condition characterized by chronic limb pain, swelling, and skin changes.
While highly effective, the AngioJet procedure, like any interventional therapy, carries potential risks. These can include vessel dissection, perforation, bradycardia (slow heart rate) due to distal embolization of adenosine (a chemical released from red blood cells during clot fragmentation), and hemolysis (red blood cell destruction) due to the high-velocity jets. Careful patient selection, skilled operator technique, and appropriate pharmacological adjuncts (e.g., heparin, antiplatelet agents) are essential to maximize benefits and minimize complications. Ongoing research continues to refine its use and explore new applications for this powerful thrombectomy technology.
Conclusion
The AngioJet thrombectomy system represents a significant advancement in the treatment of acute thrombotic events, offering a rapid and effective mechanical solution for removing debilitating and life-threatening blood clots. By harnessing the power of high-velocity saline jets and simultaneous aspiration, this device quickly restores blood flow, mitigating tissue damage and improving patient outcomes across a range of cardiovascular emergencies. As a cornerstone of modern interventional medicine, AngioJet continues to play a vital role in preventing severe complications and enhancing the quality of life for countless individuals affected by vascular thromboses.

