The image provides a detailed view of the parietal and visceral pleurae surrounding the lungs, essential components of the respiratory system. This illustration highlights the protective layers and their relationship with the chest wall and diaphragm, offering a clear understanding of lung mechanics. It serves as a valuable resource for exploring how these structures support breathing and maintain lung integrity.
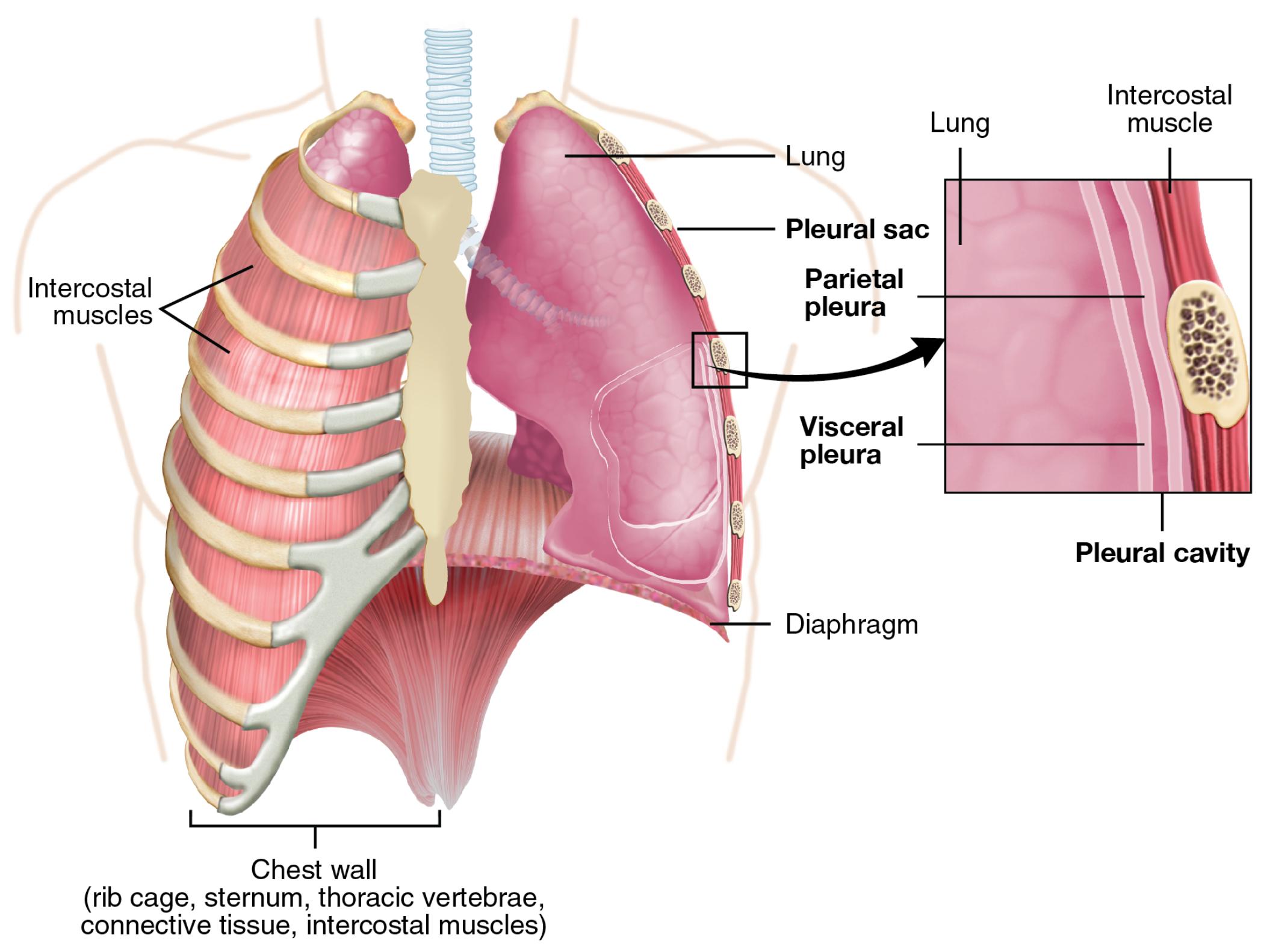
- Lung: This vital organ facilitates gas exchange, drawing oxygen into the bloodstream and expelling carbon dioxide, and is encased by the pleural membranes. Its elastic tissue allows it to expand and contract with each breath, supported by the surrounding pleurae.
- Pleural sac: This double-layered membrane encloses the lungs, creating a protective cavity that reduces friction during respiration. It consists of the parietal and visceral pleura, which work together to maintain lung function.
- Parietal pleura: This outer layer lines the chest wall, diaphragm, and mediastinum, providing a sturdy anchor for the lungs within the thoracic cavity. It produces a small amount of pleural fluid to lubricate the pleural cavity.
- Visceral pleura: This inner layer directly covers the lung surface, adhering tightly to provide support and protection during movement. It also contributes to the pleural fluid, ensuring smooth lung expansion.
- Pleural cavity: This thin space between the parietal and visceral pleura contains pleural fluid, reducing friction and allowing the lungs to move freely during breathing. It plays a critical role in maintaining negative pressure to keep the lungs inflated.
- Diaphragm: This dome-shaped muscle forms the floor of the thoracic cavity, contracting and relaxing to drive inhalation and exhalation. It works in concert with the pleural membranes to facilitate lung expansion.
- Intercostal muscles: These muscles lie between the ribs, aiding in expanding and contracting the chest wall to support breathing. They collaborate with the diaphragm to create the pressure changes needed for respiration.
- Intercostal muscle: This specific muscle group enhances rib movement, contributing to the thoracic cage’s flexibility during breathing. Its action is essential for increasing lung volume during inhalation.
- Chest wall: Composed of the rib cage, sternum, thoracic vertebrae, connective tissue, and intercostal muscles, this structure encases and protects the lungs. It provides the rigid framework necessary for respiratory mechanics.
Overview of Pleural Anatomy
The pleural anatomy depicted showcases the intricate relationship between the lungs and surrounding structures. Each component plays a unique role in ensuring efficient respiration and lung protection. This understanding is key to appreciating the respiratory system’s functionality.
- The lung serves as the primary site for gas exchange, relying on pleural support.
- Pleural sac encases the lungs, offering a protective and lubricated environment.
- The parietal pleura anchors the lungs, contributing to thoracic stability.
- Visceral pleura adheres to the lung, moving with it during respiratory cycles.
- The pleural cavity maintains a lubricating fluid layer, essential for smooth movement.
- Diaphragm drives ventilation, working with pleural pressure changes.
- Intercostal muscles assist in chest expansion, supporting inhalation.
- Intercostal muscle enhances rib cage flexibility, aiding breathing dynamics.
- The chest wall provides structural integrity, protecting the delicate lungs.
Physiological Functions of the Pleurae
The physiological roles of the pleural layers are vital for effective lung function. These structures enable the lungs to expand and contract while minimizing friction. Their coordinated action supports the respiratory process seamlessly.
- The lung expands with negative pleural pressure, drawing in air during inspiration.
- Pleural sac reduces friction, allowing the lungs to move without irritation.
- The parietal pleura secretes pleural fluid, maintaining cavity lubrication.
- Visceral pleura moves with the lung, ensuring continuous fluid distribution.
- The pleural cavity’s negative pressure keeps the lungs adhered to the chest wall.
- Diaphragm lowers to increase thoracic volume, triggering lung inflation.
- Intercostal muscles elevate ribs, expanding the chest for air intake.
- Intercostal muscle supports rib movement, enhancing ventilation efficiency.
- The chest wall stabilizes the thorax, enabling consistent breathing patterns.
Clinical Relevance and Insights
The anatomy of the parietal and visceral pleurae offers important clinical implications for respiratory health. Understanding these structures aids in diagnosing conditions like pneumothorax or pleural effusion. This knowledge is crucial for developing effective interventions.
- The lung can collapse if the pleural cavity is breached, leading to pneumothorax.
- Pleural sac inflammation, or pleuritis, can cause sharp chest pain during breathing.
- The parietal pleura’s fluid production can increase in effusion, requiring drainage.
- Visceral pleura damage may result in air leaks, complicating lung function.
- The pleural cavity’s fluid buildup can compress the lung, necessitating medical attention.
- Diaphragm dysfunction can impair ventilation, affecting pleural dynamics.
- Intercostal muscles weakness may reduce chest expansion, impacting breathing.
- Intercostal muscle strain can lead to localized pain, hindering respiration.
- The chest wall deformities, like scoliosis, can alter pleural pressure and lung capacity.
The image of the parietal and visceral pleurae provides a clear insight into their anatomical and functional significance. These layers work together to protect the lung and facilitate breathing, offering a foundation for further study. Exploring this structure enhances appreciation for the respiratory system’s resilience and the importance of maintaining pleural health.

