Mechanical thrombectomy is a revolutionary endovascular procedure used to physically remove blood clots from large blood vessels, most commonly to treat acute ischemic stroke. This minimally invasive technique involves threading specialized devices through the vascular system to entrap and extract the obstruction, restoring critical blood flow to the brain. The illustration provided demonstrates the step-by-step mechanism of a stent retriever, a specific tool designed to integrate with the thrombus for safe removal.
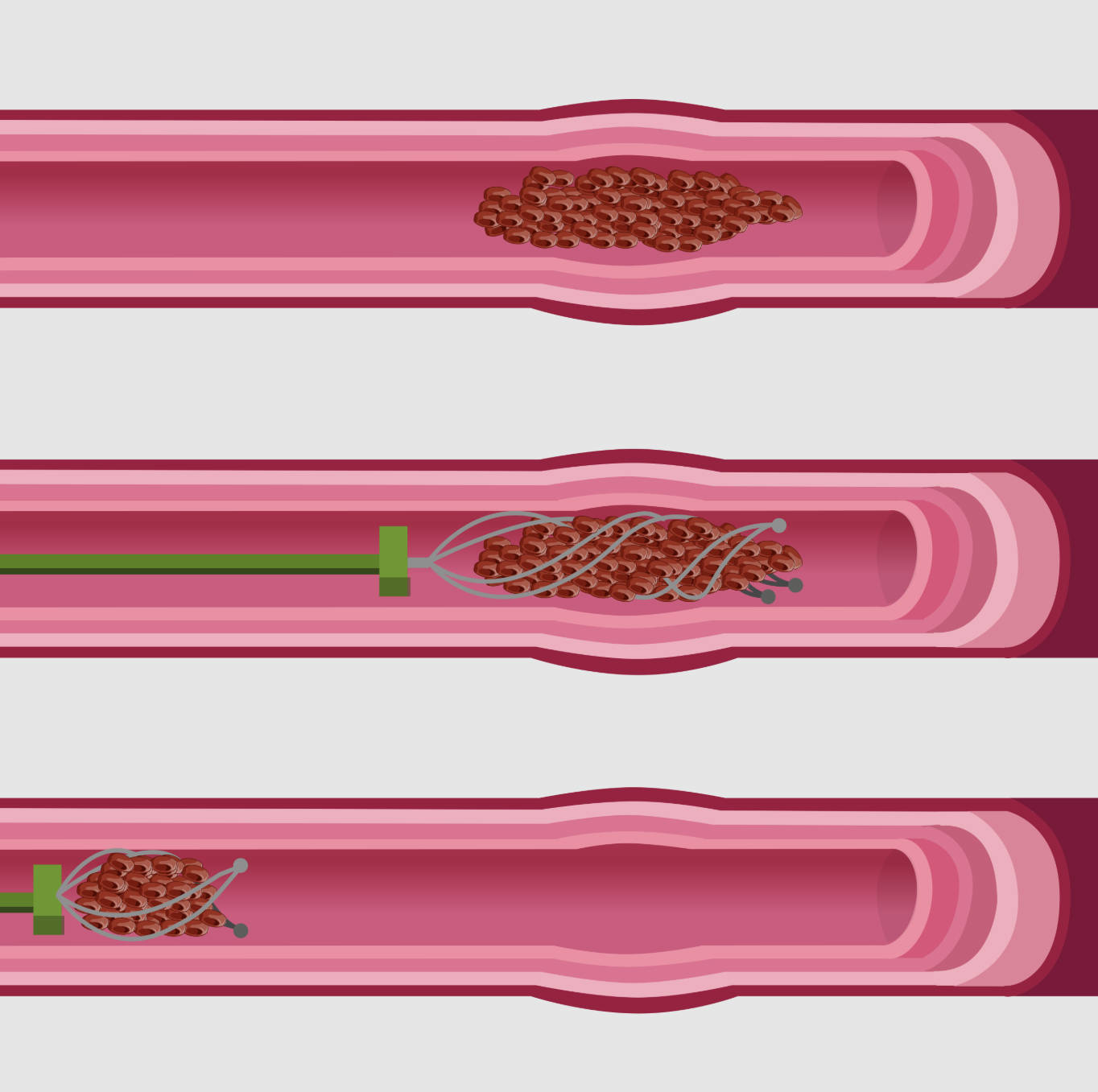
Vessel Lumen: This represents the interior channel of the artery through which blood flows. In the top panel of the illustration, the lumen is completely obstructed by a clot, preventing oxygenated blood from reaching the tissue downstream, which can lead to cellular death.
Thrombus: Also known as a blood clot, this is the dark red, aggregated mass of platelets, fibrin, and red blood cells shown blocking the vessel. In the context of a stroke, this is often an embolus that has traveled from the heart or carotid arteries and lodged in a cerebral artery.
Delivery Microcatheter: Shown as the thin green tube in the middle and bottom panels, this is a flexible medical instrument navigated through the patient’s arterial network. It serves as the conduit to deliver the retrieval device precisely to the site of the blockage without damaging the vessel walls.
Stent Retriever: This is the wire mesh structure depicted in the middle and bottom panels. It is a self-expanding device that is deployed within the clot to mesh with the fibrin strands, securing the thrombus so it can be physically pulled out of the body.
The Evolution of Acute Stroke Intervention
For decades, the only treatment for acute stroke was supportive care or systemic thrombolysis using intravenous drugs like tPA (tissue plasminogen activator). While effective for smaller clots, these drugs often fail to dissolve large blockages in major cerebral arteries. The introduction of mechanical thrombectomy has transformed the landscape of neurointerventional surgery, offering a lifeline to patients with Large Vessel Occlusions (LVO). By mechanically clearing the vessel, surgeons can restore perfusion much faster and more reliably than with medication alone.
The procedure is typically performed by a neurointerventional radiologist or neurosurgeon. Access is usually gained through the femoral artery in the groin or the radial artery in the wrist. Using fluoroscopic guidance (real-time X-ray), the surgeon navigates the catheter up to the brain. Once at the site of the occlusion, the stent retriever is deployed. This technology has significantly extended the treatment window for stroke patients, allowing interventions up to 24 hours after symptom onset in select cases.
Key advantages of mechanical thrombectomy include:
- Higher Recanalization Rates: Mechanical removal is far more successful at opening large arteries than chemical thrombolysis alone.
- Extended Time Window: It provides treatment options for patients who wake up with a stroke or arrive at the hospital outside the traditional 4.5-hour window for tPA.
- Reduced Mortality and Disability: Randomized clinical trials have consistently shown that patients treated with thrombectomy have significantly better functional independence.
Pathophysiology of Ischemic Stroke
Ischemic stroke occurs when the blood supply to a part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes. The area of dead tissue is called the core infarct, but surrounding this core is the “penumbra”—tissue that is stunned and functionally silent but structurally intact. The primary goal of the procedure shown in the image is to save the penumbra. By removing the thrombus, blood flow is restored (reperfusion), and the penumbra tissue can recover, thereby preserving speech, movement, and cognitive function.
The image specifically illustrates the “integration” and “withdrawal” phases of the procedure. When the stent retriever expands (Panel 2), it pushes the clot against the vessel wall and allows blood to temporarily flow through the mesh, which can help dissolve the clot from the inside. The struts of the stent entangle with the clot material. During withdrawal (Panel 3), the surgeon pulls the device back. This is often done in conjunction with aspiration (suction) applied through a larger catheter to ensure no fragments break off and travel further into the brain (distal embolization).
Clinical Considerations and Recovery
Not every stroke patient is a candidate for this procedure. It is specifically reserved for patients with an occlusion in the internal carotid artery, middle cerebral artery, or other large vessels. Advanced imaging, such as CT angiography or CT perfusion scanning, is used to determine if there is a salvageable penumbra. If the core infarct is already too large, restoring blood flow might cause reperfusion injury or bleeding; therefore, rapid triage and imaging are critical.
Post-procedure recovery focuses on monitoring for complications and managing blood pressure. Since the vessel has been reopened, blood pressure must be carefully controlled to prevent hemorrhage into the healing brain tissue. Patients also typically undergo a battery of tests to determine the source of the clot—such as atrial fibrillation or carotid stenosis—to prevent a recurrent event. The success of the mechanical thrombectomy is often graded using the TICI (Thrombolysis in Cerebral Infarction) scale, with a perfect score indicating complete restoration of blood flow.
Conclusion
The illustration of the stent retriever mechanism highlights the elegant engineering behind modern stroke care. By physically entrapping and removing the thrombus, medical professionals can reverse the devastating effects of cerebral ischemia. As technology advances, these devices are becoming safer and more effective, cementing mechanical thrombectomy as the standard of care for large vessel strokes and offering hope for meaningful recovery to thousands of patients annually.

