This diagram illustrates Cardiac Enhanced External Counterpulsation (EECP), a non-invasive outpatient therapy designed to improve blood flow to the heart in patients with chronic angina and heart failure. The image clearly shows a patient undergoing the procedure, highlighting the key components involved in this unique form of cardiovascular treatment. It demonstrates how external pressure is applied to the lower limbs to augment circulation.
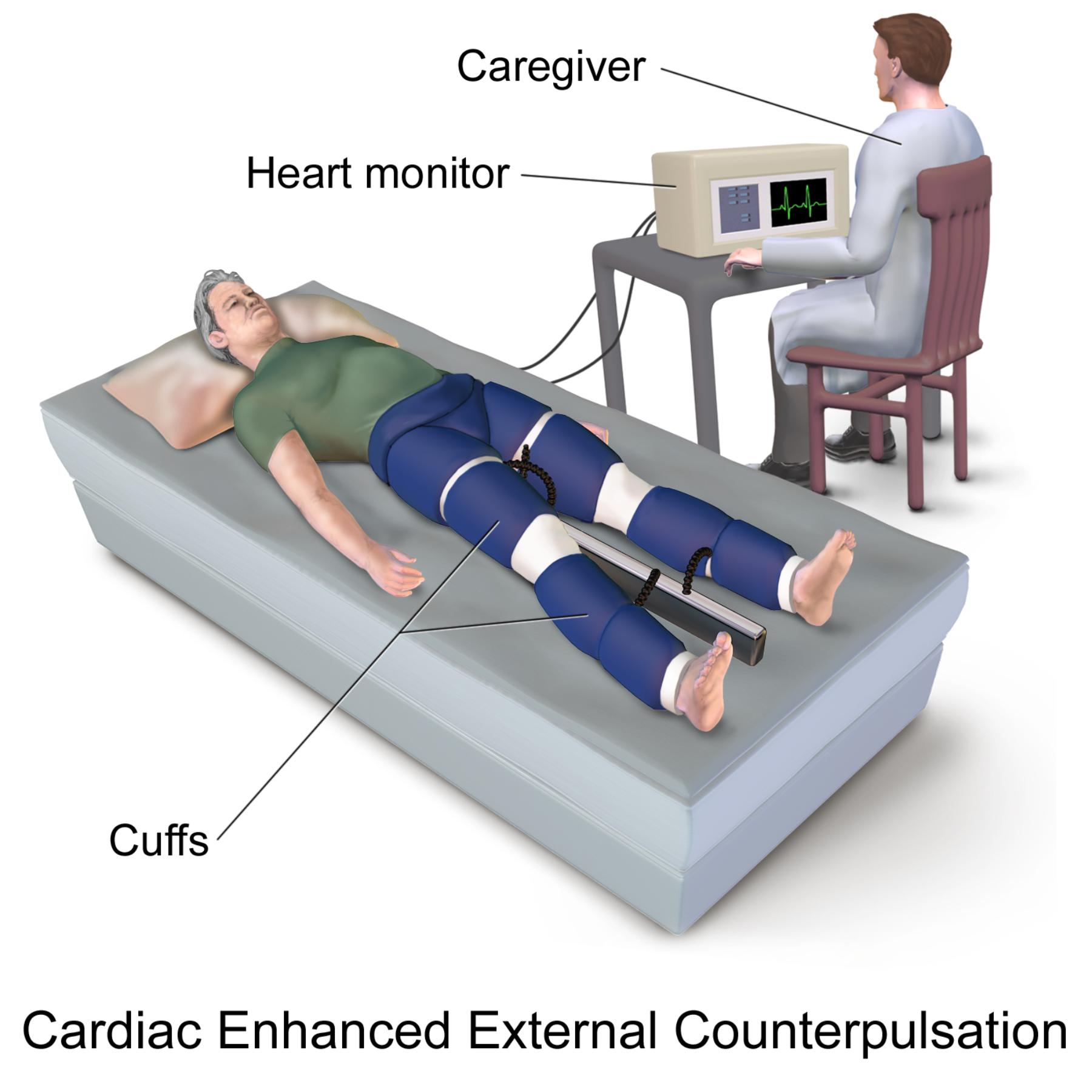
Labels Explanation:
Caregiver: A medical professional, such as a nurse or technician, who monitors the patient and operates the EECP machine during the therapy session. Their role is to ensure the patient’s comfort, adjust treatment parameters, and respond to any clinical changes.
Heart monitor: An electronic device that continuously tracks the patient’s electrocardiogram (ECG) and often their blood pressure during the EECP session. This monitoring is crucial for synchronizing the inflation and deflation of the cuffs with the patient’s cardiac cycle, ensuring optimal therapeutic effect.
Cuffs: A series of inflatable cuffs wrapped around the patient’s calves, thighs, and buttocks. These cuffs sequentially inflate and deflate in synchronization with the heartbeat, providing external compression that enhances blood flow back to the heart and throughout the coronary arteries.
Introduction to Enhanced External Counterpulsation (EECP)
Enhanced External Counterpulsation (EECP) is a non-invasive, mechanical circulatory support therapy primarily utilized for patients suffering from chronic stable angina pectoris, refractory to conventional medical therapy, or those who are not candidates for revascularization procedures like angioplasty, stenting, or bypass surgery. It is also increasingly recognized for its benefits in patients with heart failure. The core principle of EECP involves the sequential, rapid inflation and deflation of external pneumatic cuffs wrapped around the patient’s lower extremities, synchronized precisely with the cardiac cycle. This creates a “counterpulsation” effect that significantly augments blood flow to the heart.
During the diastolic phase of the cardiac cycle, when the heart muscle relaxes and fills with blood, the cuffs inflate sequentially from the calves to the thighs and buttocks. This action forcibly pushes blood from the lower extremities back towards the heart, increasing the coronary perfusion pressure and improving blood flow to the heart muscle. Immediately before systole (when the heart contracts), all cuffs rapidly deflate, creating a sudden decrease in peripheral vascular resistance. This reduction in afterload allows the heart to pump blood more easily into the systemic circulation, decreasing the workload on the heart.
EECP therapy is typically administered as an outpatient regimen, consisting of 35 one-hour sessions, usually five days a week for seven weeks. The therapy is generally well-tolerated, with most patients experiencing little to no discomfort beyond a sensation of pressure in their legs and buttocks.
The benefits of EECP stem from its ability to:
- Improve myocardial perfusion: Increase blood flow to areas of the heart muscle that were previously under-perfused due to narrowed coronary arteries.
- Stimulate angiogenesis: Promote the growth of new collateral blood vessels around blocked arteries, creating natural bypasses.
- Reduce cardiac workload: Decrease the resistance the heart has to pump against.
- Enhance endothelial function: Improve the health and function of the inner lining of blood vessels.
- Alleviate angina symptoms: Reduce the frequency and severity of chest pain.
EECP offers a promising therapeutic option for patients with chronic ischemic heart disease, providing symptomatic relief and functional improvement without the risks associated with invasive procedures.
Understanding the Physiology Behind EECP
The physiological benefits of Enhanced External Counterpulsation (EECP) are rooted in its precise interaction with the cardiovascular system, particularly during the different phases of the cardiac cycle. During diastole, the period when the heart relaxes and refills with blood, the sequential inflation of the external cuffs creates a retrograde pressure wave that travels up the arterial system. This wave significantly increases diastolic aortic pressure, which in turn drives more blood into the coronary arteries. The coronary arteries primarily receive blood during diastole, so enhancing this pressure directly improves myocardial perfusion, delivering vital oxygen and nutrients to the heart muscle, especially in areas compromised by coronary artery disease.
As the heart prepares for its next contraction (systole), the cuffs rapidly deflate. This sudden release of external pressure leads to a sharp decrease in peripheral vascular resistance, effectively creating a “vacuum” effect. The reduced afterload allows the left ventricle to eject blood more easily and efficiently, thereby reducing the heart’s workload and oxygen demand. Over time, the repeated cycles of augmented diastolic pressure and reduced systolic afterload induce a cascade of beneficial vascular adaptations. These include improved endothelial function, increased nitric oxide bioavailability (a potent vasodilator), and the stimulation of angiogenesis (the growth of new collateral blood vessels). These effects collectively contribute to alleviating angina symptoms, improving exercise tolerance, and enhancing the overall quality of life for patients with chronic ischemic heart disease.
EECP Treatment and Patient Outcomes
A typical course of EECP therapy involves 35 one-hour treatment sessions, administered once daily for approximately seven weeks. During each session, the patient lies on a treatment table while the inflatable cuffs are secured around their calves, thighs, and buttocks. An electrocardiogram (ECG) is used to monitor the heart’s electrical activity, and a finger plethysmograph measures blood flow and generates a waveform. These signals are fed into the EECP machine, which then precisely synchronizes the inflation and deflation of the cuffs with the patient’s heartbeat. The caregiver monitors these parameters and adjusts the cuff pressure to optimize the counterpulsation effect, aiming for specific hemodynamic goals.
Patients undergoing EECP therapy often experience significant improvements in their symptoms and quality of life. Studies have demonstrated that EECP can lead to a reduction in angina episodes, decreased nitroglycerin use, and an improvement in exercise capacity. These benefits can persist for several years after completing the initial course of therapy. While EECP is generally safe and well-tolerated, potential side effects are typically mild and may include skin irritation or mild discomfort under the cuffs, muscle aches, or fatigue. Contraindications for EECP include severe peripheral vascular disease, significant aortic regurgitation, severe hypertension, and active deep vein thrombosis. For many patients who have exhausted other treatment options or are not candidates for invasive procedures, EECP offers a valuable and non-invasive alternative to manage their chronic cardiac conditions effectively.
Enhanced External Counterpulsation (EECP) stands as a vital non-invasive therapy that significantly enhances cardiac function and alleviates symptoms for individuals with chronic ischemic heart disease and heart failure. By meticulously synchronizing external counterpulsation with the patient’s heartbeat, EECP improves blood flow to the heart, reduces its workload, and fosters the growth of new collateral vessels. This unique approach provides a safe and effective option, improving quality of life and functional capacity for those seeking alternatives to or complementing invasive cardiac procedures.

