This diagram visually explains the procedure of cardioversion, a medical treatment used to correct abnormally fast or irregular heartbeats (arrhythmias). It typically involves delivering a controlled electric shock to the chest to reset the heart’s electrical activity, aiming to restore a normal sinus rhythm. The image highlights the key components and personnel involved in this crucial cardiac intervention.
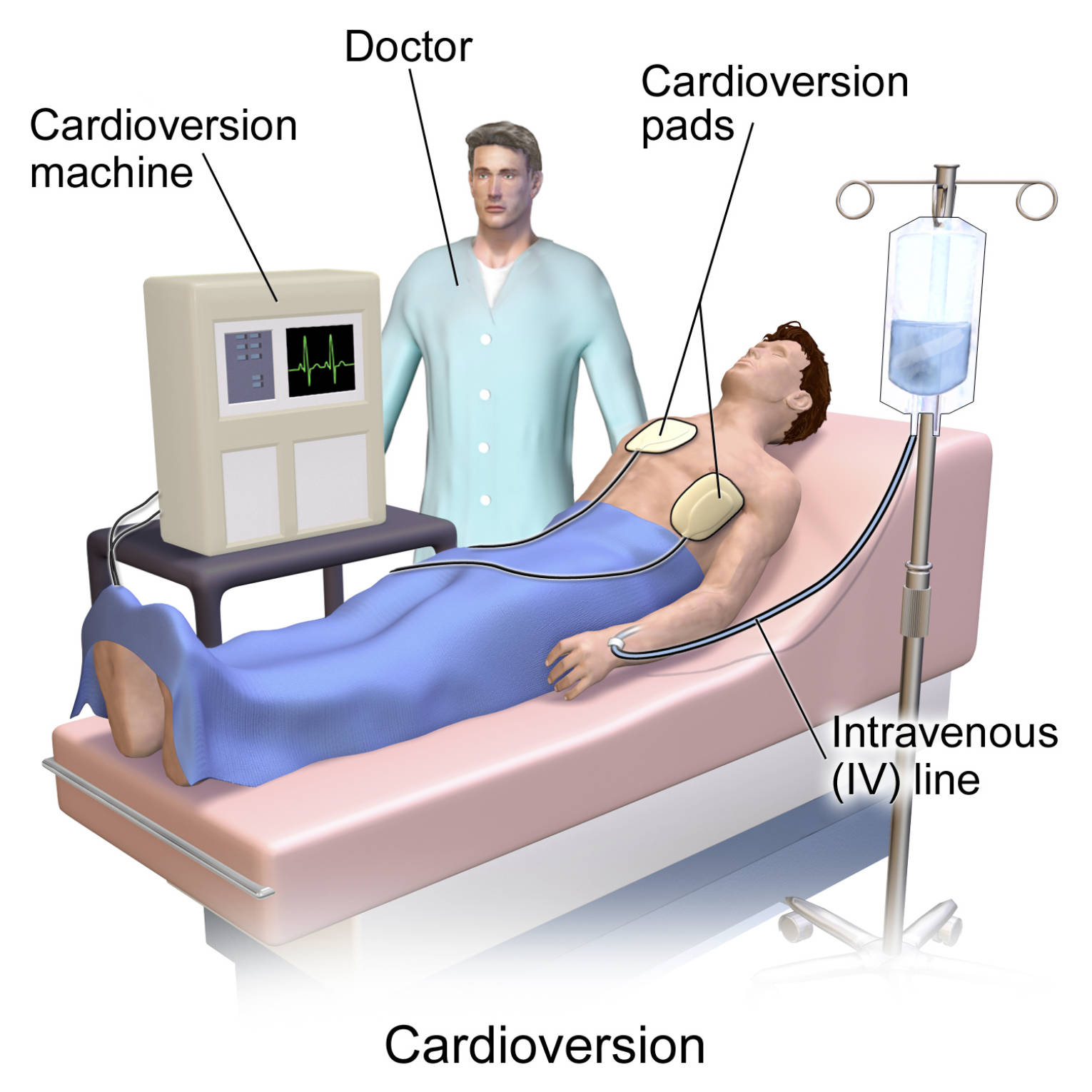
Labels Explanation:
Cardioversion machine: Also known as a defibrillator, this electronic device is central to the cardioversion procedure. It is used to deliver a precisely controlled electrical current to the heart, which helps to reset its natural rhythm and correct arrhythmias.
Doctor: A medical professional, typically a cardiologist or an emergency physician, responsible for overseeing and performing the cardioversion procedure. The doctor assesses the patient’s condition, determines the appropriate energy level, and ensures the safe and effective delivery of the electrical shock.
Cardioversion pads: These are adhesive electrodes placed on the patient’s chest and sometimes back, through which the electrical energy from the cardioversion machine is delivered to the heart. The pads ensure proper conductivity and distribution of the electrical impulse to maximize effectiveness and minimize skin irritation.
Intravenous (IV) line: A catheter inserted into a vein, typically in the arm, to administer fluids and medications directly into the bloodstream. During cardioversion, an IV line is often used to give sedatives or anesthesia to the patient, ensuring their comfort and minimizing discomfort during the procedure.
Introduction to Cardioversion
Cardioversion is a medical procedure employed to treat various types of cardiac arrhythmias, which are conditions characterized by an irregular or abnormally fast heartbeat. The heart’s electrical system, which dictates its rhythm, can sometimes malfunction, leading to palpitations, shortness of breath, dizziness, or even more severe complications like stroke or heart failure. Cardioversion aims to “reset” the heart’s electrical activity, forcing it back into a normal, synchronized rhythm. This can be achieved through two primary methods: electrical cardioversion, as depicted in the image, or pharmacological cardioversion using antiarrhythmic medications.
Electrical cardioversion involves delivering a synchronized electric shock to the chest. This brief, controlled electrical impulse momentarily depolarizes a large portion of the heart muscle cells, interrupting the abnormal electrical circuits responsible for the arrhythmia. After this brief interruption, the heart’s natural pacemaker, the sinoatrial node, typically resumes control, establishing a normal sinus rhythm. This procedure is often performed in a hospital or clinic setting and is considered a safe and effective treatment for many types of arrhythmias.
Conditions commonly treated with cardioversion include:
- Atrial fibrillation (AFib): A common arrhythmia characterized by a rapid, irregular quivering of the atria.
- Atrial flutter: A type of arrhythmia where the atria beat too fast but in a more organized pattern than AFib.
- Ventricular tachycardia (VT): A fast heart rhythm originating in the ventricles, which can be life-threatening.
- Supraventricular tachycardia (SVT): A rapid heart rhythm that originates above the ventricles.
Before undergoing electrical cardioversion, patients are usually given a sedative or light anesthesia to ensure comfort, as the electrical shock can be unpleasant. Thorough preparation, including a comprehensive medical history and evaluation, is crucial to minimize risks and optimize outcomes.
Understanding Cardiac Arrhythmias
Cardiac arrhythmias represent a broad category of conditions where the heart beats too fast (tachycardia), too slow (bradycardia), or irregularly. The heart’s rhythm is precisely controlled by an intrinsic electrical system that generates impulses, causing the heart muscle to contract and pump blood. When there is a disruption in the generation or conduction of these electrical impulses, an arrhythmia occurs. These disturbances can originate in the atria (upper chambers) or the ventricles (lower chambers) of the heart. The consequences of arrhythmias vary widely, from being benign and asymptomatic to being life-threatening.
For instance, atrial fibrillation (AFib) is a prevalent arrhythmia characterized by disorganized electrical signals in the atria, causing them to quiver instead of beating effectively. This can lead to blood pooling and clot formation, significantly increasing the risk of stroke. Ventricular tachycardia, on the other hand, involves rapid, abnormal electrical activity in the ventricles. If sustained, it can severely compromise the heart’s pumping ability, leading to a drop in blood pressure and potentially progressing to ventricular fibrillation, a chaotic electrical activity that is a common cause of sudden cardiac arrest. Understanding the specific type of arrhythmia is paramount for selecting the most appropriate treatment, which may include medications, lifestyle changes, catheter ablation, or cardioversion.
The Cardioversion Procedure and Patient Care
Before an electrical cardioversion, several preparatory steps are taken to ensure patient safety and optimize the procedure’s effectiveness. Patients are typically advised to fast for a certain period before the procedure. Blood tests, including those to check for electrolyte imbalances and thyroid function, may be performed. An echocardiogram might be done to rule out blood clots in the heart, especially for patients with atrial fibrillation, as dislodging a clot during cardioversion could lead to a stroke. Anticoagulant medication may be prescribed for several weeks before and after the procedure if a clot risk is present.
During the procedure, the patient is connected to an electrocardiogram (ECG) monitor, which continuously tracks the heart’s electrical activity. Sedation or a short-acting anesthetic is administered intravenously to ensure the patient remains comfortable and unaware of the electrical shock. The cardioversion pads are carefully placed on the chest, often one on the front and one on the back, to maximize the electrical current’s path through the heart. The doctor then delivers a synchronized electrical shock, meaning the shock is delivered precisely with the heart’s R-wave on the ECG to prevent inducing a more dangerous arrhythmia. After the shock, the medical team closely monitors the patient for the return of a normal sinus rhythm and assesses their vital signs. Patients usually recover quickly from the sedation and can often go home the same day, with instructions for post-procedure care and follow-up. Cardioversion, while generally safe, does carry some risks, including skin burns, temporary irregular rhythms, and rarely, more serious complications, which are discussed with the patient prior to the procedure.
Cardioversion is a remarkably effective tool in the cardiologist’s arsenal, offering a rapid and often successful means to restore a healthy heart rhythm for individuals struggling with various arrhythmias. By leveraging controlled electrical energy, this procedure can significantly alleviate symptoms, reduce the risk of complications like stroke, and ultimately improve the quality of life for many patients. The meticulous preparation and post-procedure care are as crucial as the shock itself, ensuring the best possible outcomes and long-term cardiac stability.

