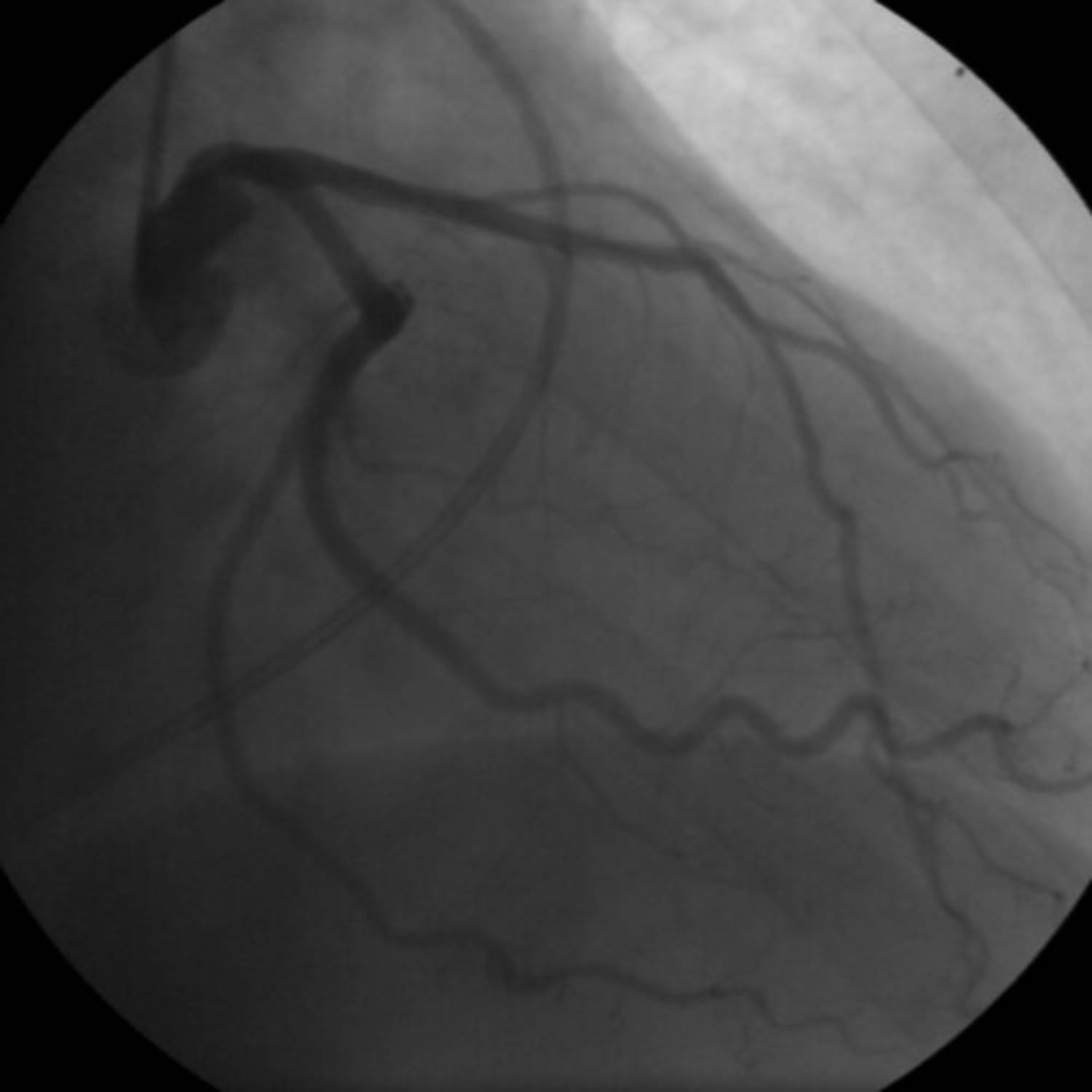
This image presents a coronary angiogram of a female patient, offering a crucial diagnostic perspective on her cardiac vasculature. Coronary angiography is an essential medical procedure used to visualize the coronary arteries, the blood vessels responsible for supplying oxygen and nutrients to the heart muscle. By using a contrast agent and X-rays, this technique allows medical professionals to detect potential blockages or narrowings that could indicate coronary artery disease (CAD) or other significant cardiac issues. This detailed view is vital for accurate diagnosis and guiding personalized treatment plans.
Introduction to Coronary Angiography in Females
Coronary angiography is a sophisticated imaging technique that plays a pivotal role in the diagnosis and management of heart conditions, particularly coronary artery disease. This procedure involves the injection of a special dye into the coronary arteries, which then become visible under X-ray imaging. The resulting angiograms, such as the one displayed, enable cardiologists to assess the patency of the arteries, identify stenoses (narrowings), and evaluate the overall blood flow to the heart muscle. While the fundamental principles of angiography remain consistent, there can be subtle differences in presentation and clinical implications between genders.
In females, symptoms of coronary artery disease can sometimes differ from those typically observed in males, often presenting atypically. This can lead to delays in diagnosis and treatment. Therefore, diagnostic tools like coronary angiography are especially important to accurately assess cardiac health. The procedure helps confirm the presence of CAD, determine its severity, and guide therapeutic decisions, which might include medication, lifestyle changes, or interventional procedures like angioplasty, stenting, or bypass surgery. The detailed visualization provided by an angiogram is indispensable for comprehensive cardiac care.
The procedure is usually performed in a cardiac catheterization laboratory by an interventional cardiologist. A thin, flexible tube called a catheter is inserted into an artery, typically in the wrist or groin, and carefully threaded to the heart. The contrast dye is then injected, highlighting the coronary arteries on an X-ray monitor. This dynamic imaging allows for real-time assessment of blood flow and identification of any abnormalities.
Key reasons a coronary angiogram might be recommended for a female patient include:
- Persistent or severe chest pain (angina) that is not responding to initial treatments.
- Symptoms of heart attack, such as sudden chest pain, shortness of breath, or pain radiating to the arm, back, neck, or jaw.
- Abnormal results on non-invasive cardiac stress tests, suggesting potential blockages.
- Evaluation before other major heart surgeries, such as valve replacement.
- New or worsening symptoms of heart failure.
These indications highlight the critical role of angiography in diagnosing and managing various cardiac conditions in women.
Understanding Coronary Artery Anatomy and CAD
The heart is supplied with oxygen-rich blood by two main coronary arteries: the left main coronary artery (LMCA) and the right coronary artery (RCA). The LMCA typically bifurcates into the left anterior descending (LAD) artery and the circumflex artery (LCx). The LAD is often referred to as the “widowmaker” due to its critical role in supplying the majority of the left ventricle, which is the heart’s main pumping chamber. It provides blood to the front and bottom of the left ventricle and the anterior two-thirds of the interventricular septum. The LCx wraps around the left side of the heart, supplying the left atrium and the posterior wall of the left ventricle. The RCA, originating from the right side, typically supplies the right atrium, right ventricle, and in most individuals, the inferior wall of the left ventricle and the posterior one-third of the interventricular septum.
Coronary artery disease (CAD) develops when plaque, made up of cholesterol, fatty substances, and other cellular material, builds up inside these arteries. This process, known as atherosclerosis, causes the arteries to narrow and harden, restricting blood flow to the heart muscle. When the heart muscle doesn’t receive enough blood, it experiences ischemia, which can lead to symptoms like angina or, in severe cases, a heart attack. Females can sometimes present with what is termed “non-obstructive CAD” or coronary microvascular dysfunction, where smaller arteries or capillaries are affected, which may not always be clearly visible on standard angiograms but can still cause significant symptoms. The image allows for direct visualization of these major vessels to identify gross obstructions.
The Angiogram Procedure and Its Diagnostic Value
During a coronary angiogram, a catheter is carefully guided to the openings of the coronary arteries. A contrast dye is then injected, making the arteries visible on X-ray screens. The rapid sequence of X-ray images, or fluoroscopy, captures the flow of the dye through the arteries, allowing the cardiologist to observe any areas where the blood flow is restricted. These restrictions, or stenoses, are often indicative of atherosclerotic plaques. The severity of these narrowings is typically measured as a percentage of the vessel’s diameter, which directly impacts treatment decisions.
The diagnostic value of an angiogram lies in its ability to precisely locate and quantify blockages. For instance, a total occlusion signifies a complete blockage, while a partial blockage may still significantly impede blood flow. In addition to identifying stenoses, an angiogram can also reveal the presence of collateral vessels—smaller blood vessels that can develop over time to bypass a blocked artery, offering some compensatory blood flow. This detailed information helps the cardiology team understand the extent of the disease and plan the most appropriate intervention, whether it’s medication adjustment, percutaneous coronary intervention (PCI) with stenting, or coronary artery bypass grafting (CABG).
Managing Coronary Artery Disease in Women
Managing coronary artery disease in women requires a comprehensive approach that considers both typical and atypical presentations. Beyond the diagnostic insights from angiography, treatment often involves a combination of lifestyle modifications and medications. Lifestyle changes include adopting a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, and quitting smoking. Pharmacological treatments commonly include statins to lower cholesterol, antihypertensive medications to control blood pressure, and antiplatelet agents like aspirin to prevent blood clot formation. When significant blockages are identified via angiography, interventional procedures such as angioplasty (using a balloon to open the artery) and stenting (placing a mesh tube to keep the artery open) are often performed. In cases of multi-vessel disease or complex blockages, coronary artery bypass grafting (CABG) may be recommended. The information gained from a coronary angiogram is thus fundamental to tailoring effective and individualized treatment strategies, ultimately aiming to improve cardiac function and patient longevity.

