Coronary Artery Disease (CAD) is a major cardiovascular condition characterized by the build-up of plaque in the heart’s arteries, leading to narrowed blood vessels and restricted blood flow. This comprehensive article delves into the core aspects of CAD, explaining its primary cause, common symptoms such as chest pain and shortness of breath, and its profound impact on heart health. Gain essential insights into this prevalent disease.
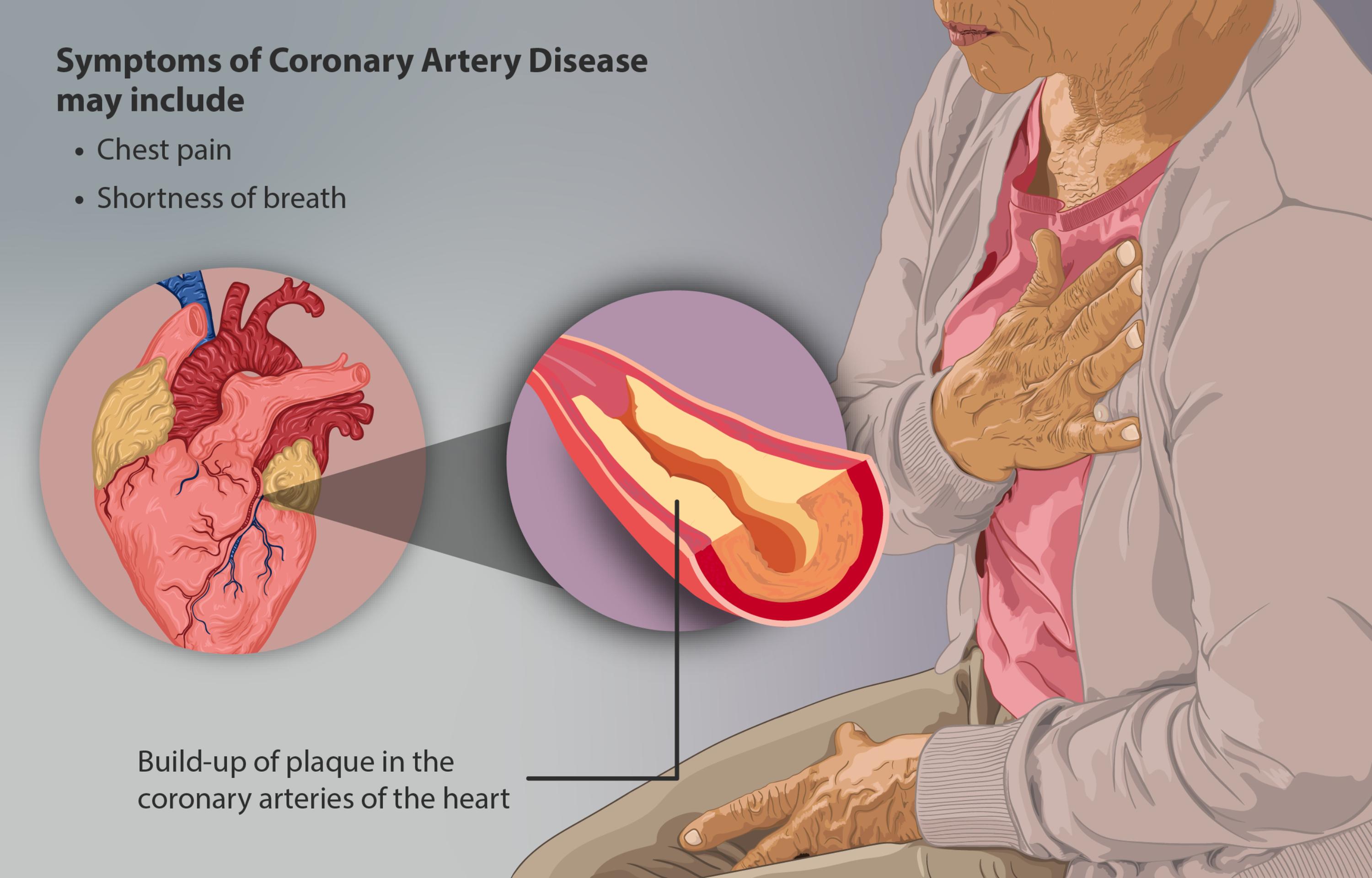
Symptoms of Coronary Artery Disease may include: This label introduces a list of common clinical manifestations that individuals might experience when suffering from CAD. These symptoms arise due to the heart muscle not receiving an adequate supply of oxygenated blood.
Chest pain: Often referred to as angina, this symptom is a hallmark of CAD and can range from a mild discomfort to a severe, crushing sensation. It typically occurs when the heart’s oxygen demand exceeds the supply, especially during physical exertion or emotional stress.
Shortness of breath: Known medically as dyspnea, this symptom occurs because the heart is struggling to pump enough blood to meet the body’s oxygen needs, or due to fluid buildup in the lungs if heart function is severely impaired. It can be particularly noticeable during activity or when lying flat.
Build-up of plaque in the coronary arteries of the heart: This describes the pathological process central to Coronary Artery Disease, where deposits of fatty substances, cholesterol, and other materials accumulate within the walls of the arteries supplying the heart. This accumulation leads to hardening and narrowing of these crucial vessels, significantly impeding blood flow.
Coronary Artery Disease (CAD) is the most common type of heart disease and a leading cause of death worldwide. It occurs when the major blood vessels that supply the heart muscle, known as the coronary arteries, become damaged and diseased. The primary culprit behind this damage is atherosclerosis, a process where plaque—a sticky substance made of fat, cholesterol, calcium, and other materials—builds up inside the arteries. This buildup causes the arteries to narrow and harden, restricting the flow of oxygen-rich blood to the heart muscle.
The image above powerfully illustrates the core problem in CAD: the obstruction of coronary arteries by plaque and the resulting symptoms experienced by an affected individual. When the heart muscle doesn’t receive enough blood and oxygen, it can’t function properly, leading to a range of symptoms that can significantly impact quality of life and, if left untreated, lead to severe complications such as heart attack, heart failure, or arrhythmias. Understanding the fundamental mechanics of plaque buildup and its physiological consequences is crucial for both prevention and effective management of this pervasive condition.
The insidious nature of Coronary Artery Disease means that it often progresses silently for many years, with individuals experiencing no symptoms in its early stages. However, as the plaque accumulates and the arteries narrow further, the demand-supply mismatch for oxygenated blood to the heart muscle becomes more pronounced, eventually leading to overt symptoms. The image’s depiction of an individual clutching their chest vividly conveys the distress associated with angina, one of the primary indicators of CAD.
The development and progression of coronary artery disease are influenced by a complex interplay of genetic predispositions and modifiable risk factors. Key modifiable risk factors include:
- High blood pressure (hypertension)
- High cholesterol levels (especially high LDL cholesterol)
- Smoking
- Diabetes
- Obesity and physical inactivity
- Unhealthy diet
Addressing these risk factors is paramount in both preventing the onset and slowing the progression of CAD.
Understanding Plaque Buildup and Its Effects
The build-up of plaque in the coronary arteries of the heart is the hallmark of Coronary Artery Disease. This process, known as atherosclerosis, begins with damage to the endothelium, the inner lining of the artery. This damage can be initiated by factors such as high blood pressure, high cholesterol, smoking, and inflammation. Once damaged, the endothelium becomes more permeable, allowing low-density lipoprotein (LDL) cholesterol particles to penetrate the arterial wall. Macrophages, a type of white blood cell, then engulf these cholesterol particles, transforming into foam cells, which are the earliest components of atherosclerotic plaque.
Over time, these foam cells accumulate, along with fibrous tissue, calcium, and other cellular debris, forming a complex plaque. As the plaque grows, it causes the artery wall to thicken and stiffen, and it encroaches upon the lumen, the open space within the artery through which blood flows. This narrowing significantly reduces the capacity of the artery to deliver oxygen-rich blood to the heart muscle, particularly during periods of increased physical activity or emotional stress when the heart’s demand for oxygen increases. This restriction in blood flow is what leads to the characteristic symptoms of CAD.
Common Symptoms of Coronary Artery Disease
The symptoms of Coronary Artery Disease typically manifest when the narrowing of the coronary arteries becomes significant enough to impede adequate blood flow to the heart muscle. The two most prominent symptoms of Coronary Artery Disease are chest pain and shortness of breath.
Chest pain, or angina, is often described as a squeezing, pressure, fullness, or aching sensation in the chest. It can also be felt in the arms (especially the left arm), neck, jaw, back, or stomach. Angina typically occurs when the heart muscle is not receiving enough oxygen (ischemia), often triggered by physical exertion, emotional stress, extreme cold, or heavy meals. The pain usually subsides with rest or medication that helps dilate the arteries, such as nitroglycerin. Unstable angina, a more severe form, can occur at rest and indicates a higher risk of heart attack.
Shortness of breath, or dyspnea, occurs when the heart’s pumping ability is compromised due to insufficient blood supply. The heart struggles to efficiently circulate blood, leading to a buildup of fluid in the lungs, which makes breathing difficult. This symptom can also be exacerbated during physical activity. In some cases, individuals may experience other symptoms such as fatigue, nausea, lightheadedness, or sweating, especially during a heart attack. Women, in particular, may experience less typical symptoms like back pain or indigestion, making diagnosis more challenging.
Diagnosis and Treatment Approaches
Diagnosing Coronary Artery Disease involves a thorough medical history, physical examination, and a range of diagnostic tests. Common tests include an electrocardiogram (ECG) to assess the heart’s electrical activity, blood tests to check cholesterol levels and other markers, and a stress test (treadmill or pharmacological) to evaluate the heart’s response to exertion. An echocardiogram provides images of the heart’s structure and function, while a coronary angiogram is considered the gold standard for directly visualizing the coronary arteries and identifying blockages.
Treatment for CAD focuses on managing symptoms, slowing disease progression, and preventing complications like heart attacks. Lifestyle modifications are fundamental and include dietary changes, regular exercise, weight management, and smoking cessation. Medications play a crucial role and may include:
- Statins: To lower cholesterol levels and stabilize plaque.
- Antiplatelet agents: Such as aspirin, to prevent blood clots.
- Beta-blockers: To reduce heart rate and blood pressure, decreasing the heart’s oxygen demand.
- ACE inhibitors/ARBs: To lower blood pressure and protect the heart.
- Nitroglycerin: To relieve angina symptoms by dilating arteries.
For significant blockages, interventional procedures or surgery may be necessary. Percutaneous coronary intervention (PCI), including angioplasty and stent placement, involves opening narrowed arteries with a balloon and inserting a stent to keep them open. Coronary artery bypass grafting (CABG) surgery creates new pathways for blood to flow around blocked arteries using grafts from other blood vessels. These interventions aim to restore adequate blood flow to the heart muscle and alleviate symptoms.
Coronary Artery Disease is a serious but manageable condition that underscores the importance of cardiovascular health. By understanding its causes, recognizing its symptoms, and adhering to appropriate preventive and therapeutic strategies, individuals can significantly reduce their risk of adverse cardiac events. Regular medical check-ups, proactive lifestyle choices, and effective management of risk factors are key to living a healthier life with or without a diagnosis of CAD.

