This article provides a comprehensive overview of dilated cardiomyopathy (DCM), a serious heart condition characterized by an enlarged and weakened heart muscle, as vividly illustrated in the provided diagram. We will compare a normal heart’s function with one affected by DCM, exploring the structural changes that impair the heart’s ability to pump blood effectively and the subsequent impact on overall cardiovascular health. This detailed explanation aims to inform both medical professionals and individuals seeking to understand this significant cardiac disease.
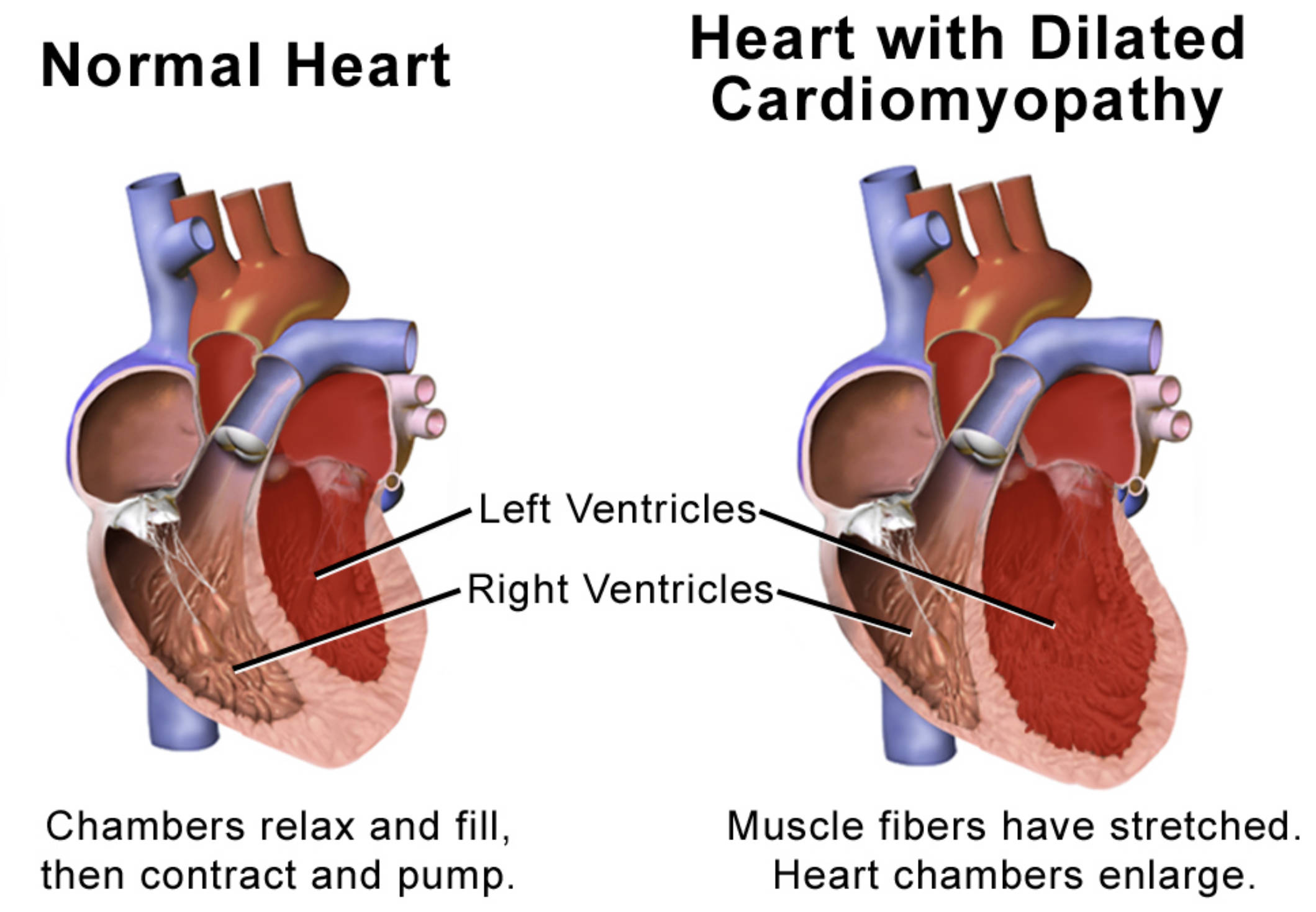
Left Ventricles: These are the primary pumping chambers responsible for ejecting oxygenated blood into the aorta for distribution throughout the body. In dilated cardiomyopathy, the left ventricle becomes significantly enlarged and its walls thin, impairing its pumping efficiency.
Right Ventricles: These chambers pump deoxygenated blood to the lungs for oxygenation. In dilated cardiomyopathy, the right ventricle may also become enlarged and weakened, further compromising the heart’s overall ability to circulate blood.
Dilated cardiomyopathy (DCM) is a type of heart muscle disease (cardiomyopathy) where the heart’s main pumping chamber, the left ventricle, becomes enlarged and weakened. This condition impairs the heart’s ability to pump blood effectively to the rest of the body, leading to a progressive decline in cardiac function. The diagram powerfully illustrates this contrast, presenting a “Normal Heart” where “Chambers relax and fill, then contract and pump” efficiently, alongside a “Heart with Dilated Cardiomyopathy” where “Muscle fibers have been stretched. Heart chambers enlarge.” This visual comparison immediately highlights the profound structural and functional abnormalities characteristic of DCM.
The enlargement and weakening of the heart muscle in DCM are not merely cosmetic changes; they have significant physiological consequences. The stretched muscle fibers result in reduced contractility, meaning the heart struggles to generate sufficient force to eject blood. This leads to a decreased ejection fraction, a key measure of the heart’s pumping efficiency, and can ultimately result in heart failure. DCM is a leading cause of heart transplantation and is associated with considerable morbidity and mortality.
Understanding the underlying mechanisms of dilated cardiomyopathy is crucial for accurate diagnosis, effective management, and potential prevention strategies. The causes of DCM are diverse, ranging from genetic predispositions to acquired factors.
- Ventricular Enlargement: The heart chambers, particularly the left ventricle, become significantly stretched and dilated.
- Impaired Contractility: The stretched muscle fibers lose their ability to contract forcefully, reducing pumping efficiency.
- Reduced Ejection Fraction: The percentage of blood pumped out with each beat decreases, indicating compromised cardiac function.
These factors underscore the serious nature of dilated cardiomyopathy and its impact on cardiovascular health.
The Pathophysiology of Dilated Cardiomyopathy
Dilated cardiomyopathy is characterized by the dilation and thinning of the ventricular walls, particularly the left ventricle, accompanied by impaired systolic function (the ability to contract and pump blood). The precise mechanisms underlying DCM are complex and multifactorial. In many cases, it is idiopathic, meaning the cause is unknown. However, known causes include genetic mutations, which account for a significant percentage of familial cases, affecting proteins involved in myocardial contractility or structural integrity. Other acquired causes include viral infections (e.g., coxsackievirus, adenovirus), which can lead to myocarditis (inflammation of the heart muscle) that progresses to DCM.
Other important etiologies include chronic alcohol abuse, certain toxic medications (e.g., some chemotherapy agents), uncontrolled hypertension, prolonged tachycardia (fast heart rate), and even peripartum cardiomyopathy, which develops during late pregnancy or shortly after childbirth. In all these scenarios, the common end result is a progressive weakening and stretching of the heart muscle fibers, as highlighted in the diagram. This stretching reduces the force of contraction, leading to a diminished stroke volume (the amount of blood pumped out per beat) and a compensatory increase in heart rate to maintain cardiac output. Over time, the chronic volume overload and impaired pumping efficiency lead to a further enlargement of the heart chambers, creating a vicious cycle that ultimately results in progressive heart failure. The enlarged left ventricles struggle to pump blood effectively, causing blood to back up into the pulmonary circulation and leading to symptoms like shortness of breath.
Clinical Manifestations and Diagnosis of DCM
The symptoms of dilated cardiomyopathy often develop gradually and can be non-specific, leading to delayed diagnosis. As the heart’s pumping ability declines, patients typically experience symptoms of heart failure. These include progressive shortness of breath, initially with exertion and later at rest; fatigue and weakness; swelling in the legs, ankles, and feet (edema); abdominal bloating; and sometimes chest pain or palpitations due to arrhythmias. The severity of symptoms often correlates with the degree of ventricular dysfunction and the extent of heart chamber enlargement. In some individuals, DCM may first be detected when an arrhythmia or a thromboembolic event (e.g., stroke) occurs.
Diagnosis of dilated cardiomyopathy involves a thorough medical history, physical examination, and a series of diagnostic tests. During a physical exam, a physician may detect an enlarged heart, abnormal heart sounds, or signs of fluid retention. An electrocardiogram (ECG) can show abnormalities in heart rhythm and evidence of ventricular enlargement. A chest X-ray typically reveals an enlarged heart silhouette and signs of pulmonary congestion. The definitive diagnostic tool is an echocardiogram, which provides real-time images of the heart’s chambers, valves, and blood flow. It allows for precise measurement of ventricular dimensions, wall thickness, and most importantly, the ejection fraction, which is often significantly reduced in DCM. Cardiac MRI can provide further detailed imaging, while blood tests may identify potential causes or assess the severity of heart failure. Genetic testing may be recommended for familial cases.
Treatment and Prognosis for Dilated Cardiomyopathy
The management of dilated cardiomyopathy focuses on alleviating symptoms, preventing disease progression, and improving the patient’s quality of life. Treatment strategies are individualized and primarily involve pharmacological therapy, lifestyle modifications, and, in advanced cases, device implantation or heart transplantation. Medications are crucial for managing DCM and heart failure. These include ACE inhibitors or angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonists (MRAs), which are proven to improve symptoms, reduce hospitalizations, and prolong life. Diuretics are used to reduce fluid retention and alleviate symptoms like swelling and shortness of breath.
For patients at risk of arrhythmias, antiarrhythmic drugs or an implantable cardioverter-defibrillator (ICD) may be necessary. Cardiac resynchronization therapy (CRT) with a specialized pacemaker can improve heart function in select patients with severe systolic dysfunction and specific conduction abnormalities. Lifestyle modifications, such as a low-sodium diet, fluid restriction, regular light exercise, and avoiding alcohol, are also vital. In cases of end-stage DCM refractory to medical therapy, heart transplantation remains the definitive treatment option, offering significantly improved survival and quality of life. Ongoing research continues to explore new therapeutic approaches and genetic therapies for DCM.

