This article presents a complex case of a neonate diagnosed with dilated cardiomyopathy (DCM) following acute deterioration. We will analyze the initial and subsequent chest X-ray findings in conjunction with clinical and laboratory data, offering insights into the presentation, diagnosis, and management of this critical condition in infants for medical students and practitioners.
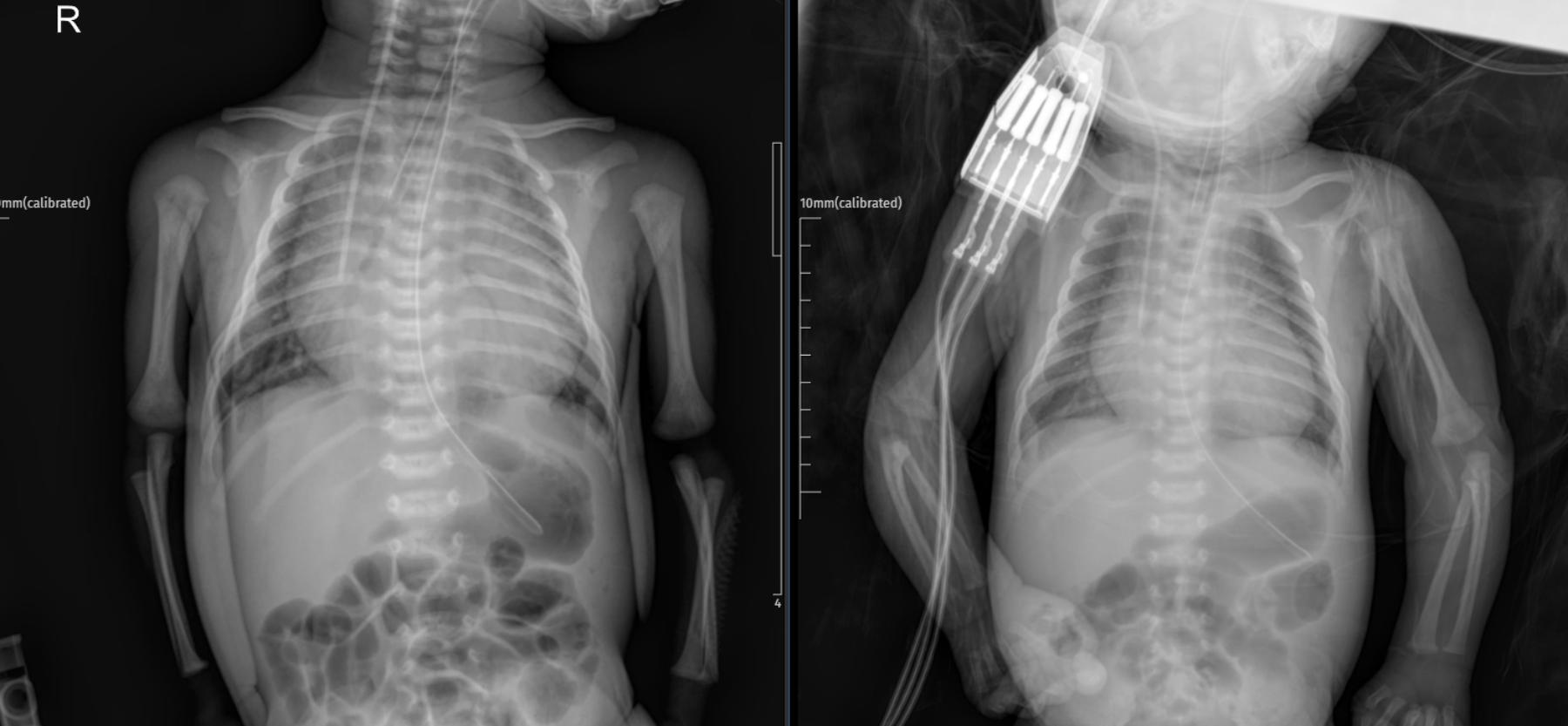
- Left Image (Admission X-ray): A supine anteroposterior chest and abdominal radiograph of a neonate, showing an endotracheal tube in place and a nasogastric tube extending into the stomach. The cardiac silhouette appears enlarged with an increased cardiothoracic index. The lung fields show mild vascular congestion.
- Right Image (ICU Day 2 X-ray): A follow-up supine anteroposterior chest and abdominal radiograph, showing similar findings with the endotracheal tube and nasogastric tube in position. The cardiac silhouette remains enlarged. There is evidence of an intravenous line stabilizer on the right arm.
Clinical Presentation
A male infant, born at 41 weeks gestation with a birth weight of 3580 grams via normal spontaneous delivery, presented on postnatal day 27.
- History from Parents: On November 11, 2025, (postnatal day 26) at approximately 10:00 PM, about 3 hours after receiving gas drops, the parents noticed decreased movements, reduced feeding, and perioral cyanosis. They subsequently sought care at an external medical center.
- Initial Presentation at External Center: The infant was evaluated as having a poor general condition, with arterial blood gas revealing a pH of 6.85. The patient was intubated with a 3.5 Fr endotracheal tube and referred to our facility.
Emergency Department & Initial Radiological Findings
Upon arrival at the emergency department, a PA chest X-ray was performed.
- PA Chest X-ray Interpretation (Left Image): The chest X-ray showed an increased cardiothoracic index, indicative of cardiomegaly. This finding prompted an urgent consultation with pediatric cardiology.
- Pediatric Cardiology Assessment: Following the consultation, a preliminary diagnosis of dilated cardiomyopathy (DCM) was made. The infant was admitted to the Pediatric Intensive Care Unit (PICU) for further investigation and treatment.
Initial Physical Examination (Admission to PICU)
- General condition: Poor, intubated, sedated.
- Skin: Normal, no rash.
- Head-Neck: No cervical lymphadenopathy. Anterior and posterior fontanelles open, normal fullness, normal width.
- Oropharynx: Normal.
- Respiratory System: Harsh inspiratory and expiratory breath sounds, dyspnea, no rales, no rhonchi, no wheezing, no intercostal retractions (due to intubation).
- Cardiovascular System: S1+ S2+, no extra sounds, no murmurs heard, peripheral pulses palpable bilaterally.
- Gastrointestinal System: Abdomen soft, no defense, no rebound tenderness, gas and stool passage present.
- Genitourinary System: Externally male, no hernia, no major urogenital anomaly.
- Neuromuscular System: Pupils isocoric, light reflex +/+.
- Extremities: No deformities.
PICU Course (Day 2 – November 13, 2025)
The infant, now on postnatal day 29, is in the PICU for the second day with a preliminary diagnosis of dilated cardiomyopathy.
- Current Status: General condition poor, intubated, sedated.
- Physical Examination: Largely unchanged from admission, with normal skin, head, and neck findings. Respiratory and cardiovascular systems remain monitored. Urine output is present.
- Fluid Balance: +130 mL, urine output rate: 2.9 mL/kg/hr.
- Ventilator Settings (SIMV-BD-BK mode): P’: 19/17, PEEP: 6, Respiratory Rate: 42, Trigger flow: 2, I:E Ratio: 1:2, T.insp: 5%, Breath period: 1.4, FiO2: 25%.
- Morning Arterial Blood Gas: pH: 7.32, pCO2: 52.4 mmHg, HCO3: 23.3 mmol/L, Na: 130.0 mmol/L, K: 3.95 mmol/L, Cl: 100 mmol/L, Ca: 1.00 mmol/L, Glucose: 85 mg/dL, Lactate: 1.44 mmol/L.
- Nutrition: Infant formula or breast milk, with proper doses.
Treatment Plan
- Aspirin: With proper doses via nasogastric tube.
- Furosemide: With proper doses intravenously.
- Acetazolamide: With proper doses (to be given 6 hours apart from furosemide, not concurrently).
- Midazolam: With proper doses via continuous intravenous infusion.
- Fentanyl: With proper doses via continuous intravenous infusion.
- Dobutamine: With proper doses via continuous intravenous infusion.
Note: The dosages of sedation and inotropic agents are dynamically adjusted based on the patient’s clinical status.
Please note: Drug types and dosages should be verified according to your country’s relevant pharmaceutical dosage guidelines, or by consulting a licensed physician in the relevant department.
Further Investigations & Management Plans
- Respiratory tract swab sample taken.
- Consultation with Pediatric Metabolism and Medical Genetics.
- Pediatric Metabolism Consultation (November 14, 2025, 14:00): Noted the patient’s acute onset of respiratory distress and deterioration. Confirmed dilated cardiomyopathy on echocardiogram (AST=70, CK=300). Recommended comprehensive metabolic investigations including tandem mass spectrometry, organic acids in urine, amino acids in urine/serum, very long-chain fatty acids, and homocysteine. Re-consultation with results is advised.
- Medical Genetics Consultation: Requested blood samples (2 purple top, 1 dry green top) and advised parents to bring family members for a genetic consultation on Monday.
- Pediatric Cardiology Consultation (November 13, 2025, 10:00): Diagnosed dilated cardiomyopathy with significant left ventricular enlargement, moderate mitral regurgitation (MR), tricuspid regurgitation (TR), and an ejection fraction (EF) of 26%. Initiated milrinone, furosemide, and aspirin. Recommended admission to a neonatal intensive care unit.
Conclusion
This case of neonatal dilated cardiomyopathy highlights a critical and often rapidly progressive condition in infants. The initial chest X-ray demonstrating cardiomegaly was crucial in guiding the diagnostic pathway, which was further confirmed by echocardiography revealing severe left ventricular dysfunction. The acute presentation with metabolic acidosis and subsequent intubation underscores the severity of the disease. The ongoing investigations into metabolic and genetic etiologies are paramount, given the family history of consanguinity and the need to identify the underlying cause for long-term management and genetic counseling.
This content is for educational and reference purposes only and should not be used as a basis for diagnosis or treatment. Always consult with a qualified healthcare professional for any medical concerns.

