The human bladder is a remarkable organ, playing a crucial role in the urinary system. This article delves into the intricate bladder anatomy, exploring its various components and their functions, alongside a microscopic view of its tissue structure. Understanding these aspects is key to comprehending urinary health and potential conditions.
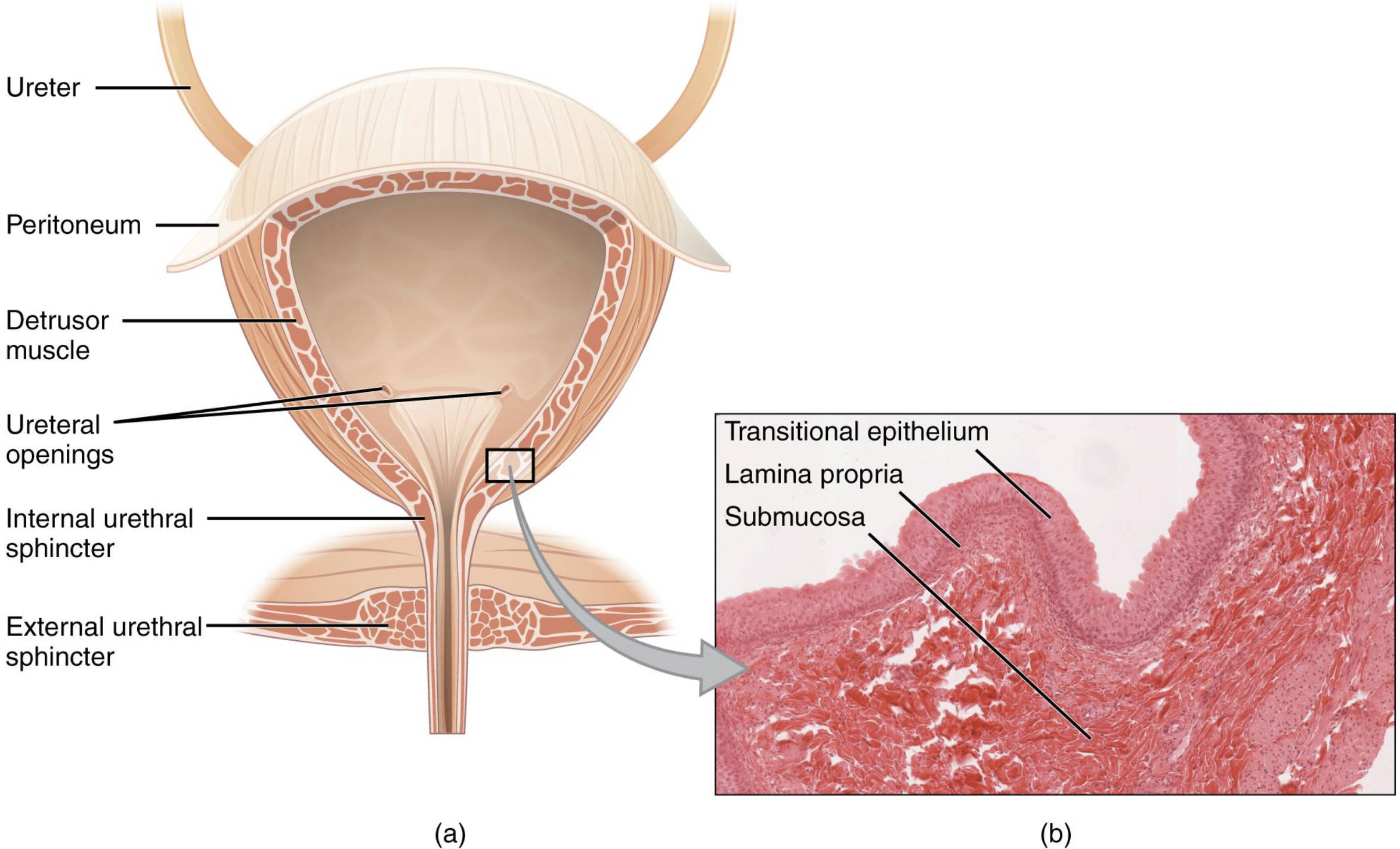
Ureter: These muscular tubes transport urine from the kidneys to the bladder. Peristaltic contractions of the ureter walls ensure a continuous, one-way flow of urine, preventing backflow and protecting the kidneys from infection.
Peritoneum: This serous membrane lines the abdominal cavity and covers the superior surface of the bladder. It helps to anchor the bladder in place and reduces friction between organs.
Detrusor muscle: This smooth muscle forms the main wall of the bladder and is responsible for its contraction during urination. Its coordinated action expels urine from the bladder into the urethra.
Ureteral openings: These are the entry points where the ureters connect to the bladder, allowing urine to enter. Their angled insertion into the bladder wall acts as a functional valve, preventing vesicoureteral reflux.
Internal urethral sphincter: This involuntary smooth muscle sphincter is located at the bladder neck, where it meets the urethra. It normally remains contracted to prevent urine leakage and relaxes during urination under parasympathetic control.
External urethral sphincter: This voluntary skeletal muscle sphincter is located distal to the internal sphincter, surrounding the urethra. It allows conscious control over the flow of urine, enabling us to hold urine until an appropriate time for micturition.
The bladder is a hollow, muscular, and distensible organ that serves as a temporary reservoir for urine. Situated in the pelvic cavity, its size and position vary depending on the amount of urine it contains. The ability of the bladder to store urine and then efficiently expel it is vital for maintaining fluid and electrolyte balance in the body and for preventing infections. Its intricate design, from macroscopic structures to microscopic cellular arrangements, reflects its complex physiological role.
The bladder’s function is meticulously controlled by both the autonomic and somatic nervous systems, allowing for both involuntary storage and voluntary voiding of urine.
- Storage Phase: During this phase, the detrusor muscle is relaxed, and the internal and external urethral sphincters are contracted. This allows the bladder to fill with urine without leakage.
- Voiding Phase: When the bladder reaches a certain capacity, stretch receptors send signals to the brain, initiating the urge to urinate. If appropriate, the detrusor muscle contracts, and the sphincters relax, leading to the expulsion of urine.
The histology of the bladder wall reveals several distinct layers, each contributing to its unique function. The innermost layer is the transitional epithelium, also known as urothelium, which is remarkably adapted for distension. This specialized stratified epithelium can thin out as the bladder fills, preventing rupture and leakage. Beneath the transitional epithelium lies the lamina propria, a layer of connective tissue rich in blood vessels, nerves, and lymphatic vessels that nourish the overlying epithelium. The submucosa, a thicker layer of connective tissue, supports the mucosa and contains additional blood vessels and nerves. The most prominent layer is the detrusor muscle, a complex network of smooth muscle fibers arranged in various directions, enabling the bladder to contract powerfully from multiple angles during urination. The outermost layer is the serosa, or adventitia, which provides protection and anchoring.
Understanding the bladder’s anatomy and histology is not only fundamental for general medical knowledge but also crucial for diagnosing and treating various urinary conditions. Conditions such as urinary incontinence, urinary tract infections, and bladder overactivity often stem from dysfunctions in one or more of these anatomical or histological components. For example, issues with the detrusor muscle can lead to difficulties in emptying the bladder, while weakening of the urethral sphincters can result in involuntary urine leakage. Further research into these intricate structures continues to enhance our understanding and improve patient care.

