The menstrual cycle is a dynamic and meticulously choreographed process essential for female reproduction and overall health. This comprehensive diagram provides a detailed timeline, illustrating the intricate correlation between hormonal fluctuations and the physiological changes occurring in the ovaries and uterus. Understanding these phases and their hormonal drivers is fundamental to comprehending fertility, contraception, and various aspects of women’s reproductive health.
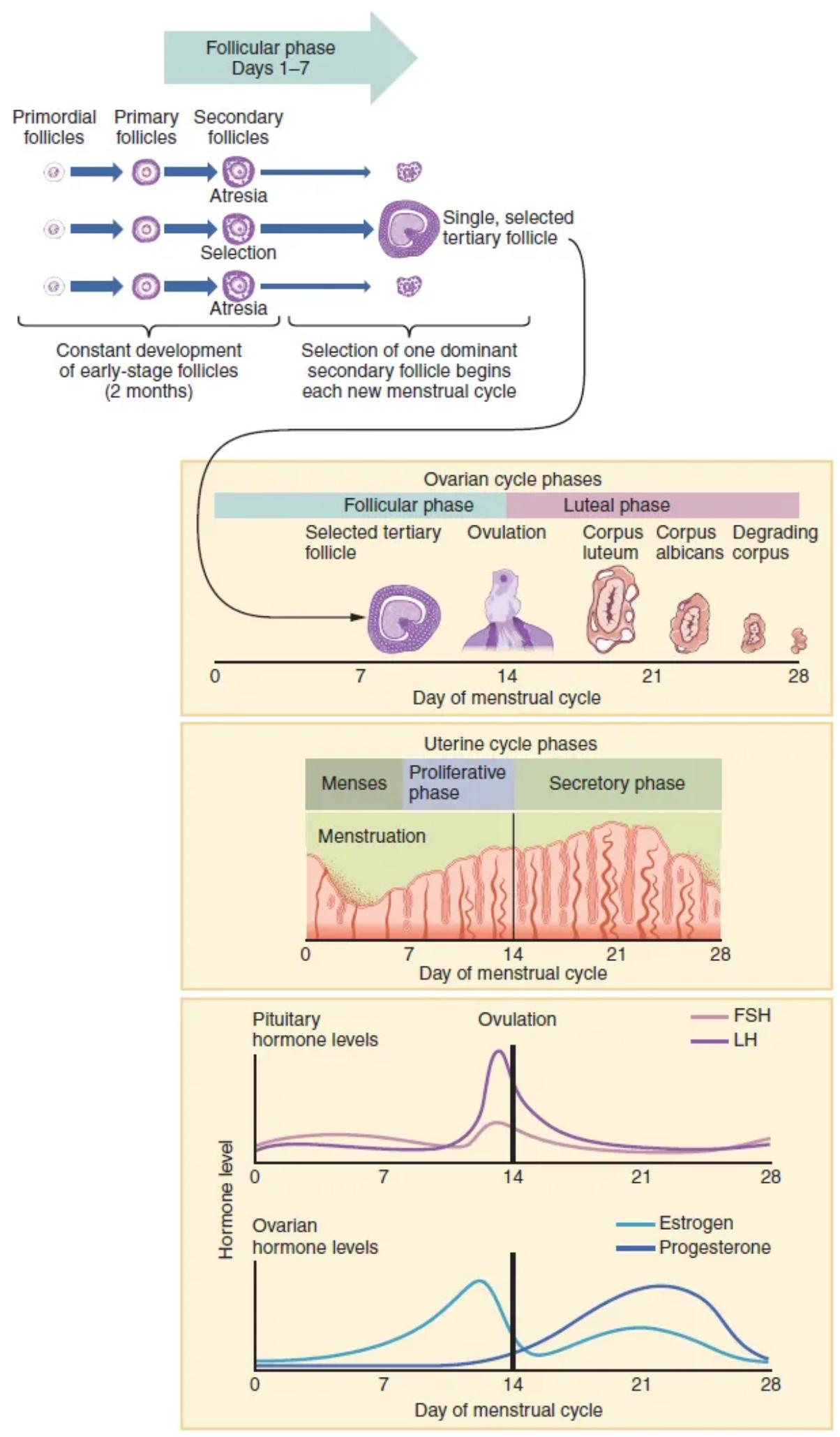
Follicular phase: The follicular phase is the first phase of the ovarian cycle, spanning from day 1 to ovulation (typically around day 14). During this phase, several ovarian follicles grow under the influence of FSH, with one dominant follicle eventually selected for maturation.
Primordial follicles: Primordial follicles are the earliest and most numerous stage of ovarian follicles, consisting of a primary oocyte surrounded by a single layer of flattened granulosa cells. These dormant follicles represent the ovarian reserve a female is born with.
Primary follicles: Primary follicles develop from primordial follicles, characterized by an enlarged oocyte and cuboidal granulosa cells. A zona pellucida also begins to form around the oocyte.
Secondary follicles: Secondary follicles are distinguished by multiple layers of granulosa cells and the appearance of theca cells around the follicle. These follicles continue to grow, producing increasing amounts of estrogen.
Selection: This refers to the process during the follicular phase where one of the growing secondary follicles is chosen to become the dominant follicle. This dominant follicle will be the one to fully mature and ovulate, while others undergo atresia.
Atresia: Atresia is the process of degeneration and resorption of ovarian follicles that do not reach full maturation. The vast majority of follicles, even those that begin to develop, will undergo atresia at various stages.
Single, selected tertiary follicle: After selection, the dominant secondary follicle rapidly develops into a single, large tertiary (antral) follicle. This follicle contains a fluid-filled antrum and is poised for ovulation.
Constant development of early-stage follicles (2 months): This highlights that the development of follicles from primordial to early antral stages is a continuous, asynchronous process that takes approximately two months. This means follicles preparing for ovulation in one cycle began their development several cycles prior.
Selection of one dominant secondary follicle begins each new menstrual cycle: While early follicle development is constant, the final selection of one dominant follicle to proceed to ovulation is a key event that occurs at the beginning of each new menstrual cycle, driven by hormonal cues.
Ovarian cycle phases: The ovarian cycle describes the changes occurring in the ovarian follicles themselves. It is divided into two main phases: the follicular phase (follicle growth) and the luteal phase (corpus luteum formation and regression).
Luteal phase: The luteal phase is the second phase of the ovarian cycle, occurring after ovulation and typically lasting from day 14 to day 28. It is characterized by the formation and activity of the corpus luteum, which secretes progesterone.
Selected tertiary follicle: This represents the single dominant follicle that has matured and is ready for ovulation, containing a large antrum and a healthy oocyte. It is often referred to as a Graafian follicle.
Ovulation: Ovulation is the process where the mature ovarian follicle ruptures, releasing the secondary oocyte from the ovary into the fallopian tube. This event typically occurs around day 14 of a 28-day cycle, triggered by the LH surge.
Corpus luteum: The corpus luteum is a temporary endocrine structure that forms from the remnants of the ruptured follicle after ovulation. It produces large amounts of progesterone and some estrogen, essential for preparing and maintaining the uterine lining.
Degrading corpus: If pregnancy does not occur, the corpus luteum begins to degrade around 10-14 days after ovulation. This degradation leads to a sharp decline in progesterone and estrogen levels.
Corpus albicans: The corpus albicans is the white, fibrous scar tissue that remains in the ovary after the complete degeneration of the corpus luteum. It marks the end of a luteal phase where pregnancy did not occur.
Day of menstrual cycle: This represents the timeline, typically a 28-day cycle, against which all ovarian, uterine, and hormonal events are charted. Day 1 conventionally marks the start of menstruation.
Uterine cycle phases: The uterine cycle describes the cyclical changes occurring in the endometrium (lining) of the uterus. It is divided into three phases: menses, proliferative phase, and secretory phase.
Menses: Menses, or menstruation, is the shedding of the functional layer of the uterine endometrium, typically lasting from day 1 to day 5-7 of the menstrual cycle. It occurs due to the withdrawal of progesterone and estrogen.
Proliferative phase: The proliferative phase is the stage of the uterine cycle during which the endometrium rapidly rebuilds and thickens. It occurs concurrently with the follicular phase of the ovarian cycle, driven primarily by rising estrogen levels.
Secretory phase: The secretory phase is the stage of the uterine cycle following ovulation, during which the endometrium becomes highly glandular and vascularized, secreting nutrients. This phase is driven by progesterone from the corpus luteum, preparing the uterus for embryo implantation.
Pituitary hormone levels: This graph illustrates the cyclical changes in the concentrations of hormones released by the anterior pituitary gland, namely FSH and LH, throughout the menstrual cycle.
FSH: The graph shows FSH (Follicle-Stimulating Hormone) levels, which are elevated during the early follicular phase to stimulate follicle growth. Its levels decline mid-cycle due to negative feedback but may show a small surge around ovulation.
LH: The graph depicts LH (Luteinizing Hormone) levels, which are crucial for the ovarian cycle. A massive surge in LH around day 14 is the definitive trigger for ovulation.
Ovulation: Indicated by a vertical line around day 14, ovulation is the release of the mature oocyte from the dominant follicle. It is directly preceded by the LH surge and marks the transition from the follicular to the luteal phase.
Ovarian hormone levels: This graph illustrates the cyclical changes in the concentrations of hormones released by the ovaries, namely estrogen and progesterone, throughout the menstrual cycle.
Estradiol: The graph shows estradiol (a type of estrogen) levels, which rise significantly during the follicular phase due to production by the growing follicles. A peak in estradiol triggers the LH surge.
Progesterone: The graph depicts progesterone levels, which remain low during the follicular phase and rise sharply after ovulation during the luteal phase. Progesterone is primarily produced by the corpus luteum to prepare the uterus for pregnancy.
The Choreography of Female Reproduction
The female menstrual cycle is a sophisticated biological rhythm that orchestrates a monthly preparation for potential pregnancy. It is a finely tuned interplay between the central nervous system, the pituitary gland, and the ovaries, resulting in cyclical changes that affect both the ovary (ovarian cycle) and the uterus (uterine cycle). This intricate process, typically spanning 28 days, is fundamental to understanding female fertility, hormonal health, and the mechanisms behind various reproductive conditions. The detailed timeline presented in the diagram elucidates how fluctuating hormone levels drive specific physiological events, leading to the maturation and release of an egg, and the readiness of the uterine lining for implantation.
The cycle begins with the shedding of the uterine lining, known as menses, and simultaneously initiates the growth of new ovarian follicles. This initial phase sets the stage for the selection of a single dominant follicle, which will eventually release its oocyte. The entire system is a prime example of a complex neuroendocrine feedback loop, where hormones produced by one gland influence the activity of others, ensuring a coordinated and precise sequence of events.
Key events and hormonal drivers of the menstrual cycle include:
- The follicular phase of the ovary, driven by FSH and estrogen.
- The proliferative phase of the uterus, stimulated by estrogen.
- The LH surge, triggering ovulation around day 14.
- The luteal phase of the ovary, characterized by the corpus luteum and progesterone.
- The secretory phase of the uterus, maintained by progesterone.
Disruptions in this delicate hormonal balance can lead to irregularities, anovulation, or infertility, emphasizing the critical importance of a well-functioning reproductive axis.
Interconnected Phases and Hormonal Control
The menstrual cycle commences with the follicular phase of the ovarian cycle and the menses of the uterine cycle. During the early follicular phase, Follicle-Stimulating Hormone (FSH) from the anterior pituitary stimulates the growth of several early-stage follicles (primordial, primary, and secondary). As these follicles grow, they produce increasing amounts of estrogen, primarily estradiol. Estradiol, during this phase, primarily exerts negative feedback on the hypothalamus and pituitary, reducing FSH and LH secretion, which helps in the selection of a single dominant follicle. Concurrently, high estrogen levels trigger the proliferative phase in the uterus, causing the endometrium to thicken and repair after menstruation.
As the dominant follicle matures, its production of estradiol peaks. This high level of estradiol switches from negative to positive feedback on the hypothalamus, leading to a surge in Gonadotropin-Releasing Hormone (GnRH). The increased GnRH, in turn, causes a massive surge in Luteinizing Hormone (LH) from the anterior pituitary, which is the definitive trigger for ovulation. Ovulation, typically occurring around day 14, marks the transition to the luteal phase of the ovarian cycle and the secretory phase of the uterine cycle. After the oocyte is released, the remnants of the ruptured follicle transform into the corpus luteum under the influence of LH. The corpus luteum then becomes the primary producer of progesterone, along with some estrogen. Progesterone is crucial for maintaining the thickened, secretory endometrium, making it receptive for potential embryo implantation. If pregnancy does not occur, the corpus luteum degenerates around day 24-26, leading to a sharp decline in progesterone and estrogen. This hormonal withdrawal causes the functional layer of the endometrium to slough off, initiating menstruation and marking the start of a new cycle.
In conclusion, the menstrual cycle is a precisely regulated biological event driven by a complex interplay of pituitary and ovarian hormones. Each phase—follicular, ovulatory, and luteal—is characterized by distinct hormonal profiles and corresponding physiological changes in the ovaries and uterus. A thorough understanding of this hormonal orchestration is paramount for comprehending female reproductive physiology, diagnosing and managing conditions like irregular periods or infertility, and informing family planning strategies.

