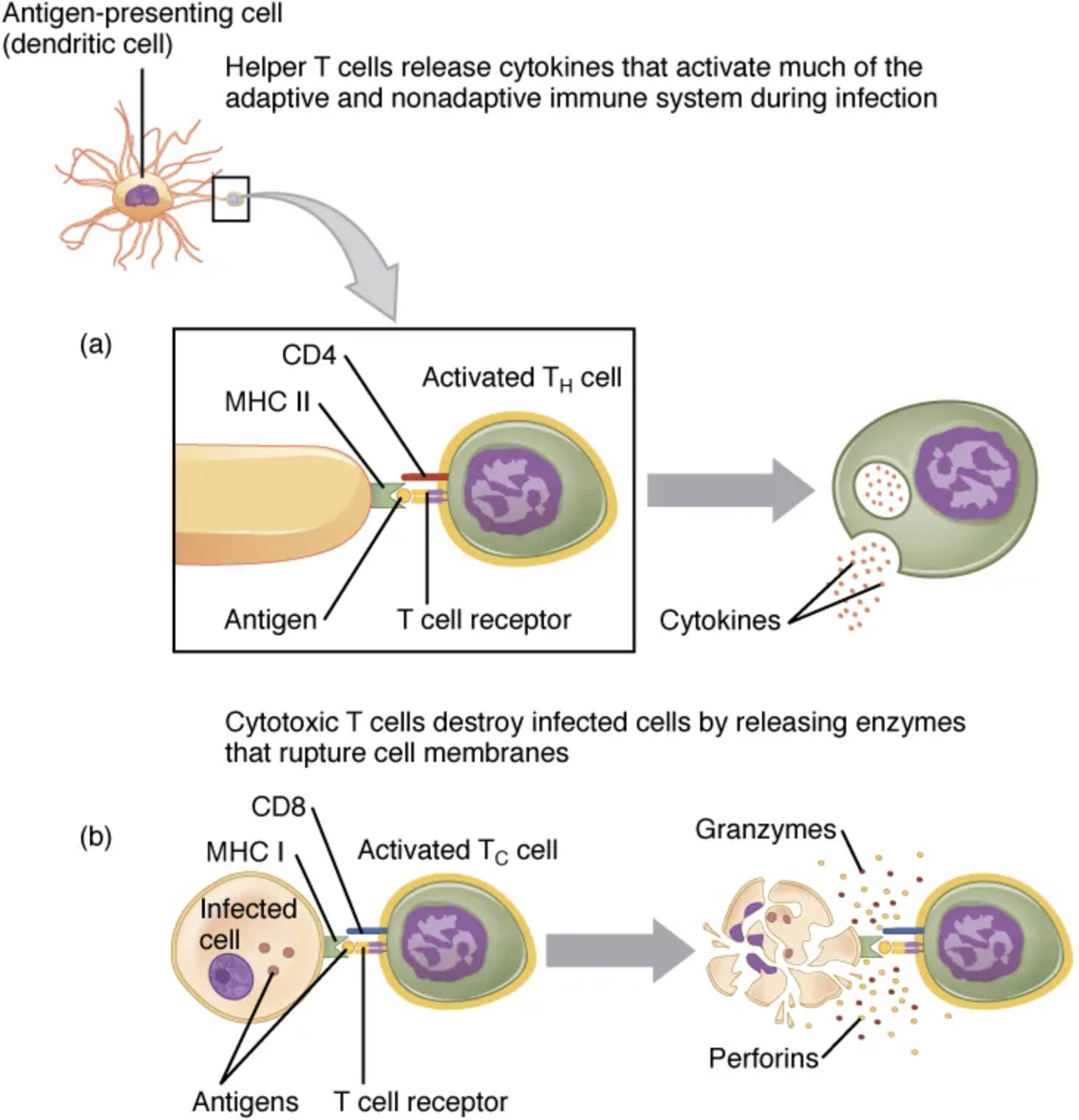
Pathogen presentation is a vital process that enables the immune system to detect and combat infections by displaying pathogen-derived antigens to T cells, guided by the major histocompatibility complex (MHC) molecules. This mechanism involves CD4+ helper and regulatory T cells interacting with extracellular pathogens via MHC class II, while CD8+ cytotoxic T cells target intracellular pathogens through MHC class I, as illustrated in this detailed image. This visual guide offers a clear perspective on how these interactions drive effective immune responses.
Labeled Components of Pathogen Presentation
Extracellular pathogen: This microbe, such as bacteria, resides outside cells and is engulfed by antigen-presenting cells. It is processed into peptides for presentation on MHC class II molecules.
Intracellular pathogen: This pathogen, like viruses, replicates inside host cells and is degraded into peptides within the cell. Its fragments are presented on MHC class I molecules.
Antigen-presenting cell (APC): Cells like dendritic cells or macrophages capture and process extracellular pathogens. They display antigens on their surface to activate T cells.
MHC class II molecule: Found on APCs, this molecule binds peptides from extracellular pathogens in its binding cleft. It presents these peptides to CD4+ T cells to initiate helper responses.
MHC class I molecule: Present on nearly all nucleated cells, this molecule binds peptides from intracellular pathogens. It displays them to CD8+ T cells for cytotoxic action.
CD4 molecule: This co-receptor on helper and regulatory T cells strengthens the interaction with MHC class II-peptide complexes. It enhances T cell activation and cytokine production.
CD8 molecule: Located on cytotoxic T cells, this co-receptor binds to MHC class I-peptide complexes. It boosts the T cell’s ability to recognize and destroy infected cells.
Helper T cell: Activated by MHC class II presentation, this CD4+ cell releases cytokines to coordinate immune responses. It supports B cells and other immune effectors.
Regulatory T cell: Also CD4+, this cell modulates the immune response to prevent overactivity. It helps maintain tolerance and prevent autoimmunity.
Cytotoxic T cell: This CD8+ cell recognizes MHC class I-peptide complexes on infected cells. It induces apoptosis to eliminate the pathogen-infected cell.
Peptide fragment (extracellular): Derived from processed extracellular pathogens, this peptide is loaded onto MHC class II. It serves as the specific antigen recognized by CD4+ T cells.
Peptide fragment (intracellular): Generated from degraded intracellular pathogens, this peptide binds to MHC class I. It is presented to CD8+ T cells for immune targeting.
Cell membrane: The outer layer of the APC or infected cell where MHC-peptide complexes are displayed. It facilitates T cell recognition and activation.
Cytokines: These signaling molecules, released by helper T cells, amplify the immune response. They recruit and activate additional immune cells.
Anatomical Context of Pathogen Presentation
Pathogen presentation occurs across various cell types, linking innate and adaptive immunity.
- Extracellular pathogens are internalized by APCs for processing.
- Intracellular pathogens are degraded within infected cells.
- MHC class II molecules on APCs present extracellular peptides.
- MHC class I molecules on all cells display intracellular peptides.
- CD4 and CD8 molecules enhance T cell-MHC binding.
- Helper, regulatory, and cytotoxic T cells respond at the cell membrane.
This illustration showcases the cellular landscape of immune recognition.
Physiological Role in Immune Defense
Pathogen presentation drives targeted immune responses against diverse threats.
- Antigen-presenting cells process extracellular pathogens, loading peptides onto MHC class II.
- Infected cells degrade intracellular pathogens, presenting peptides via MHC class I.
- CD4+ helper T cells activate upon MHC class II recognition, releasing cytokines.
- CD8+ cytotoxic T cells target MHC class I-presented peptides, killing infected cells.
- Regulatory T cells modulate the response, preventing excessive inflammation.
- Peptide fragments ensure specific antigen targeting by T cells.
This process ensures a balanced and effective immune attack.
Mechanisms of MHC Class Interaction
MHC molecules employ distinct pathways for pathogen presentation.
- MHC class II binds extracellular peptides in endosomal compartments.
- MHC class I loads intracellular peptides in the endoplasmic reticulum.
- CD4 enhances helper T cell activation by stabilizing MHC class II binding.
- CD8 strengthens cytotoxic T cell recognition of MHC class I complexes.
- Antigen-presenting cells optimize peptide presentation for T cell engagement.
- Cytokines amplify the signal, recruiting additional immune support.
These mechanisms highlight the precision of immune targeting.
Clinical Relevance of Pathogen Presentation
Understanding this process aids in managing immune-related conditions.
- MHC class II defects can lead to impaired CD4+ T cell responses, increasing infection risk.
- MHC class I dysfunction may reduce CD8+ T cell activity, aiding viral persistence.
- CD4+ T cell depletion, as in HIV, weakens helper functions.
- CD8+ T cell failures are linked to cancer immune evasion.
- Regulatory T cell overactivity can suppress immunity, promoting tumors.
- Cytokine imbalances are studied in autoimmune diseases like rheumatoid arthritis.
This knowledge supports innovative diagnostic and therapeutic strategies.
Developmental and Adaptive Features
Pathogen presentation adapts to the body’s evolving immune needs.
- Antigen-presenting cells mature, enhancing peptide processing over time.
- MHC molecules develop genetic diversity, broadening antigen coverage.
- CD4 and CD8 co-receptors refine their function with immune experience.
- Helper and cytotoxic T cells gain specificity through antigen exposure.
- Regulatory T cells evolve to balance immunity and tolerance.
- Cytokine production adjusts to the intensity of pathogen challenges.
This adaptability ensures robust protection against varied threats.
Pathogen presentation, as illustrated, is a cornerstone of immune defense, with MHC class I and II molecules displaying antigens to engage CD4+ and CD8+ T cells effectively. By coordinating helper, regulatory, and cytotoxic responses, this process exemplifies the body’s ability to adapt and respond to pathogens, making it a compelling focus for exploring immune health and resilience.


good
this information is satisfactory
this is satisfactory