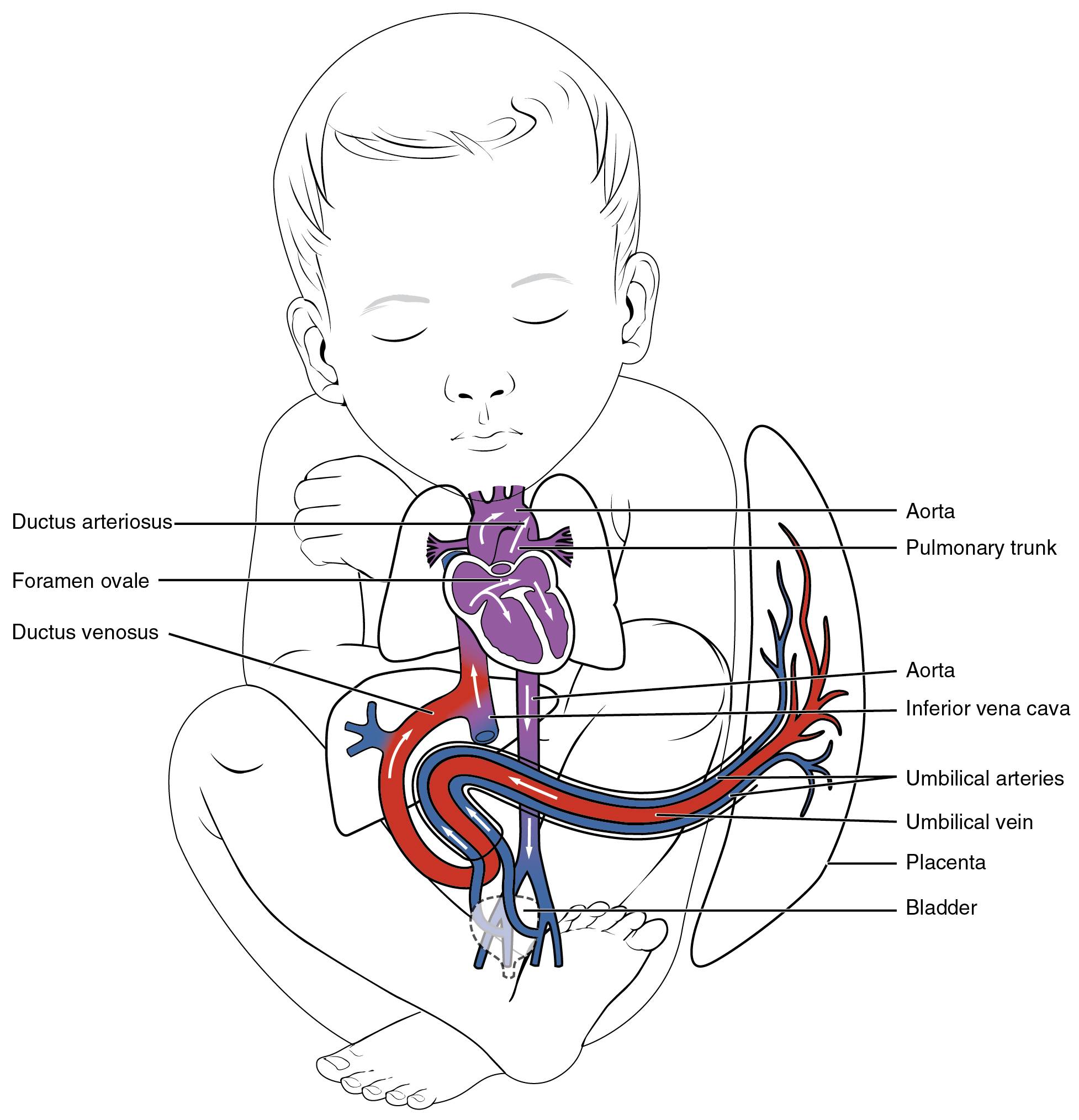
The circulatory system of a fetus features unique shunts that allow blood to bypass the lungs and liver, adapting to prenatal life where oxygen is supplied by the placenta. These temporary structures, including the foramen ovale, ductus arteriosus, and ductus venosus, ensure efficient oxygen delivery to vital organs until birth triggers their closure. Exploring this anatomy provides a deeper appreciation of how the fetal cardiovascular system supports development before transitioning to postnatal circulation.
Detailed Anatomy of Labeled Structures
The following sections detail each labeled component of the fetal shunt system, outlining its role and location.
Ductus arteriosus: The ductus arteriosus is a temporary vessel connecting the pulmonary trunk to the aorta, allowing blood to bypass the undeveloped lungs during fetal life. It closes shortly after birth as lung function begins, becoming the ligamentum arteriosum.
Foramen ovale: The foramen ovale is an opening in the interatrial septum that permits blood flow from the right atrium to the left atrium, bypassing the pulmonary circulation. It typically seals after birth due to changes in pressure, forming the fossa ovalis.
Ductus venosus: The ductus venosus links the umbilical vein to the inferior vena cava, shunting oxygenated blood from the placenta through the liver. It closes after birth as placental circulation ceases, becoming the ligamentum venosum.
Aorta: The aorta carries oxygenated blood from the left ventricle to the body, receiving additional flow via the ductus arteriosus in the fetus. It supports systemic circulation, adapting postnatally as shunts close.
Pulmonary trunk: The pulmonary trunk transports deoxygenated blood from the right ventricle, with much of its flow diverted through the ductus arteriosus in utero. It becomes the primary route to the lungs after birth.
Inferior vena cava: The inferior vena cava returns blood from the lower body and placenta to the right atrium, mixing with shunted blood from the ductus venosus. It plays a key role in directing blood flow toward the foramen ovale.
Umbilical arteries: The umbilical arteries carry deoxygenated blood from the fetus to the placenta for oxygenation, branching from the internal iliac arteries. They regress after birth into the medial umbilical ligaments.
Umbilical vein: The umbilical vein transports oxygenated blood from the placenta to the fetus, entering via the umbilical cord and connecting to the ductus venosus. It closes after birth, becoming the ligamentum teres.
Placenta: The placenta serves as the fetal lung and nutrient source, oxygenating blood that enters the umbilical vein and removing waste via the umbilical arteries. It is essential for fetal growth until delivery.
Bladder: The bladder is anatomically related to the umbilical arteries, which pass nearby before reaching the placenta. It remains functional postnatally as the urinary system matures.
Physiological Role of Fetal Shunts
Fetal shunts are critical for adapting circulation to prenatal conditions, ensuring oxygen delivery to the brain and heart.
- The ductus arteriosus diverts blood from the pulmonary trunk to the aorta, reducing lung workload since fetal lungs are fluid-filled.
- The foramen ovale allows right-to-left atrial flow, prioritizing blood to the left side of the heart for systemic circulation.
- The ductus venosus bypasses the liver, directing oxygenated blood from the umbilical vein to the inferior vena cava for efficient delivery.
- These shunts close at birth as the lungs inflate and placental circulation stops, transitioning to adult circulation patterns.
Clinical Relevance and Developmental Changes
Understanding fetal shunts aids in recognizing congenital issues and monitoring postnatal adjustments.
- Persistent ductus arteriosus after birth can lead to a heart murmur, requiring medical intervention like catheter closure.
- An unclosed foramen ovale may result in an atrial septal defect, potentially causing long-term circulatory strain.
- The ductus venosus closure is typically complete within weeks, with failure linked to rare vascular anomalies.
- Regular prenatal ultrasounds monitor umbilical arteries and vein flow, ensuring proper placental function.
Integration with Postnatal Circulation
Fetal shunts integrate with the broader circulatory system, adapting seamlessly after birth.
- The aorta and pulmonary trunk realign their flow as the ductus arteriosus closes, directing blood to the lungs.
- The inferior vena cava adjusts as the ductus venosus shuts, relying on hepatic circulation for blood processing.
- Hormonal changes, such as a surge in catecholamines, trigger umbilical arteries and vein closure post-delivery.
- The placenta detaches, shifting oxygen supply to the lungs, with the bladder unaffected by these circulatory changes.
In conclusion, the fetal shunt system, including the ductus arteriosus, foramen ovale, and ductus venosus, is a remarkable adaptation that supports prenatal life. A thorough understanding of these structures encourages awareness of their transition at birth, promoting healthy developmental outcomes.

