The regulation of arteriole smooth muscle and veins is a complex process that ensures proper blood flow and pressure throughout the body. This table outlines the neural, endocrine, and other factors that influence vasoconstriction and vasodilation, providing a comprehensive view of how the circulatory system maintains balance.
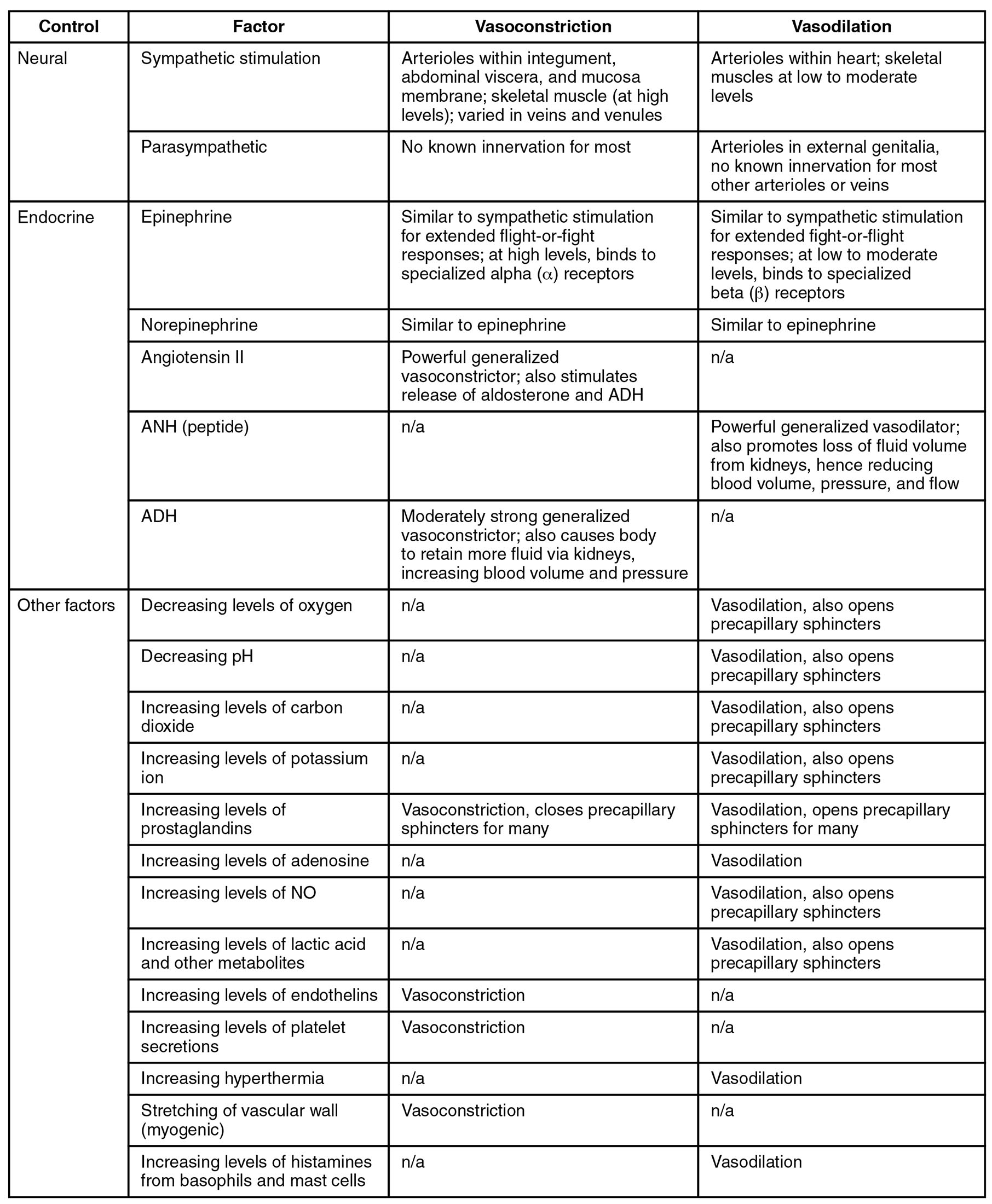
Control This category encompasses the primary systems regulating vascular tone. It includes neural and endocrine mechanisms that dictate blood vessel behavior.
Factor These are the specific stimuli or substances triggering vascular responses. They range from nervous system inputs to hormonal signals and environmental changes.
Recommended Study Resource
Gray's Anatomy: The Anatomical Basis of Clinical Practice
Enhance your anatomical knowledge with Gray's Anatomy: The Anatomical Basis of Clinical Practice. This authoritative text offers in-depth insights and illustrations, perfect for medical students and practitioners aiming for clinical excellence.
At AnatomyNote.com, we offer free resources on anatomy, pathology, and pediatric medicine for medical students and professionals. Purchasing through our Amazon links, like Gray's Anatomy, supports our server costs and content creation at no additional cost to you.
Disclosure: As an Amazon Associate, we earn a commission from qualifying purchases.
Disclosure: As an Amazon Associate, we earn a commission from qualifying purchases at no extra cost to you.
Vasoconstriction This process narrows blood vessels, increasing resistance and blood pressure. It is mediated by various factors affecting arteriole smooth muscle and veins differently.
Vasodilation This process widens blood vessels, reducing resistance and enhancing blood flow. It targets specific regions to meet metabolic demands or external conditions.
Neural Under this control, the nervous system modulates vessel diameter. It involves sympathetic and parasympathetic influences on circulation.
Sympathetic stimulation This activates arteriole smooth muscle in the integument, abdomen, and skeletal muscle to constrict. It also varies in veins, aiding in blood pressure regulation during stress.
Anatomy Flash Cards
Master anatomy with detailed, exam-ready flash cards.
AnatomyNote.com offers free anatomy and pathology resources. Your purchase of Anatomy Flash Cards supports our site at no extra cost.
As an Amazon Associate, we earn from qualifying purchases.
Parasympathetic This has minimal impact on most vessels, with no known innervation for vasoconstriction. It promotes vasodilation in external genitalia and some other areas.
Endocrine Hormones from this system play a significant role in vascular tone. They interact with specific receptors to induce constriction or dilation.
Epinephrine This hormone mimics sympathetic effects, causing vasoconstriction during fight-or-flight responses. It also induces vasodilation in heart and skeletal muscles via beta receptors.
Norepinephrine Similar to epinephrine, it promotes vasoconstriction in many vessels. It also supports vasodilation in specific areas with beta receptor activity.
Angiotensin II A powerful vasoconstrictor, it stimulates the release of aldosterone and ADH. It has no known vasodilation effect in this context.
ANH (peptide) This atrial natriuretic hormone causes generalized vasodilation. It reduces blood volume, pressure, and flow from the kidneys.
ADH This antidiuretic hormone strongly induces vasoconstriction to retain fluid. It increases blood volume and pressure via kidney action.
Other factors Environmental and metabolic changes also influence vascular tone. These factors complement neural and endocrine controls.
Decreasing levels of oxygen Low oxygen levels do not cause vasoconstriction. They trigger vasodilation, opening precapillary sphincters to enhance oxygen delivery.
Decreasing pH A drop in pH has no vasoconstrictive effect. It leads to vasodilation, opening precapillary sphincters to improve circulation.
Increasing levels of carbon dioxide Elevated carbon dioxide does not constrict vessels. It causes vasodilation, opening precapillary sphincters for better perfusion.
Increasing levels of potassium ion High potassium levels lack a vasoconstrictive response. They result in vasodilation, opening precapillary sphincters.
Increasing levels of prostaglandins These can cause vasoconstriction, closing precapillary sphincters in some cases. They also induce vasodilation, opening sphincters in other instances.
Increasing levels of adenosine Adenosine does not cause vasoconstriction. It promotes vasodilation, opening precapillary sphincters.
Increasing levels of NO Nitric oxide has no vasoconstrictive effect. It leads to vasodilation, opening precapillary sphincters.
Increasing levels of lactic acid and other metabolites These metabolic byproducts do not constrict vessels. They cause vasodilation, opening precapillary sphincters to support tissue needs.
Increasing levels of endothelins Endothelins induce vasoconstriction in affected vessels. They have no known vasodilatory effect.
Increasing levels of platelet secretions These secretions cause vasoconstriction. They lack a vasodilatory response.
Increasing hyperthermia Elevated body temperature does not cause vasoconstriction. It results in vasodilation to aid heat dissipation.
Stretching of vascular wall (myogenic) This mechanical stress induces vasoconstriction. It has no vasodilatory effect.
Increasing levels of histamines from basophils and mast cells Histamines do not cause vasoconstriction. They promote vasodilation to support inflammatory responses.
Neural Control of Vascular Tone
Arteriole smooth muscle responds dynamically to neural inputs for precise regulation. Sympathetic and parasympathetic systems play distinct roles in this process.
- Sympathetic stimulation constricts arterioles in the skin and abdomen during stress.
- Parasympathetic effects are limited, mainly dilating vessels in the genitalia.
- This balance ensures blood is redirected to vital organs as needed.
- Neural control acts rapidly, complementing slower hormonal responses.
- Overactivation of sympathetic tone can lead to hypertension.
Endocrine Influences on Blood Vessels
Hormones like epinephrine and angiotensin II exert powerful effects on vascular tone. These endocrine factors target specific receptors for tailored responses.
- Epinephrine causes vasoconstriction in most areas but dilates heart vessels.
- Angiotensin II boosts blood pressure by constricting arterioles and veins.
- ADH strengthens vasoconstriction to retain fluid and raise pressure.
- ANH counteracts these effects, promoting vasodilation to reduce volume.
- Hormonal imbalances can disrupt normal circulatory function.
Other Factors Affecting Vasoconstriction and Vasodilation
Metabolic and environmental factors significantly influence arteriole smooth muscle behavior. These triggers adapt circulation to tissue demands.
- Decreasing oxygen levels open sphincters to improve oxygen supply.
- Increasing carbon dioxide dilates vessels to remove metabolic waste.
- Prostaglandins can either constrict or dilate based on local needs.
- Hyperthermia induces vasodilation to regulate body temperature.
- These responses ensure tissues receive adequate perfusion under stress.
Clinical Relevance of Vascular Regulation
Understanding these mechanisms aids in managing circulatory health effectively. The interplay of factors supports both normal and pathological states.
- Vasoconstriction from endothelins is targeted in treating pulmonary hypertension.
- Vasodilation from nitric oxide is harnessed in erectile dysfunction therapies.
- Imbalances in prostaglandin levels affect inflammatory conditions.
- Myogenic responses help diagnose vascular stiffness in aging.
- This knowledge guides interventions for conditions like shock or edema.
The regulation of arteriole smooth muscle and veins through neural, endocrine, and other factors highlights the body’s adaptive capacity. This intricate system ensures blood pressure and flow are maintained, offering a foundation for exploring circulatory health and potential treatments.




