Maintaining blood glucose concentration within the optimal range of 70 mg/dL to 110 mg/dL is essential for energy balance and overall health, achieved through a finely tuned homeostatic mechanism. This article explores a diagram illustrating how insulin lowers blood glucose when levels rise and how glucagon increases it when levels drop, providing a clear understanding of this critical physiological process.
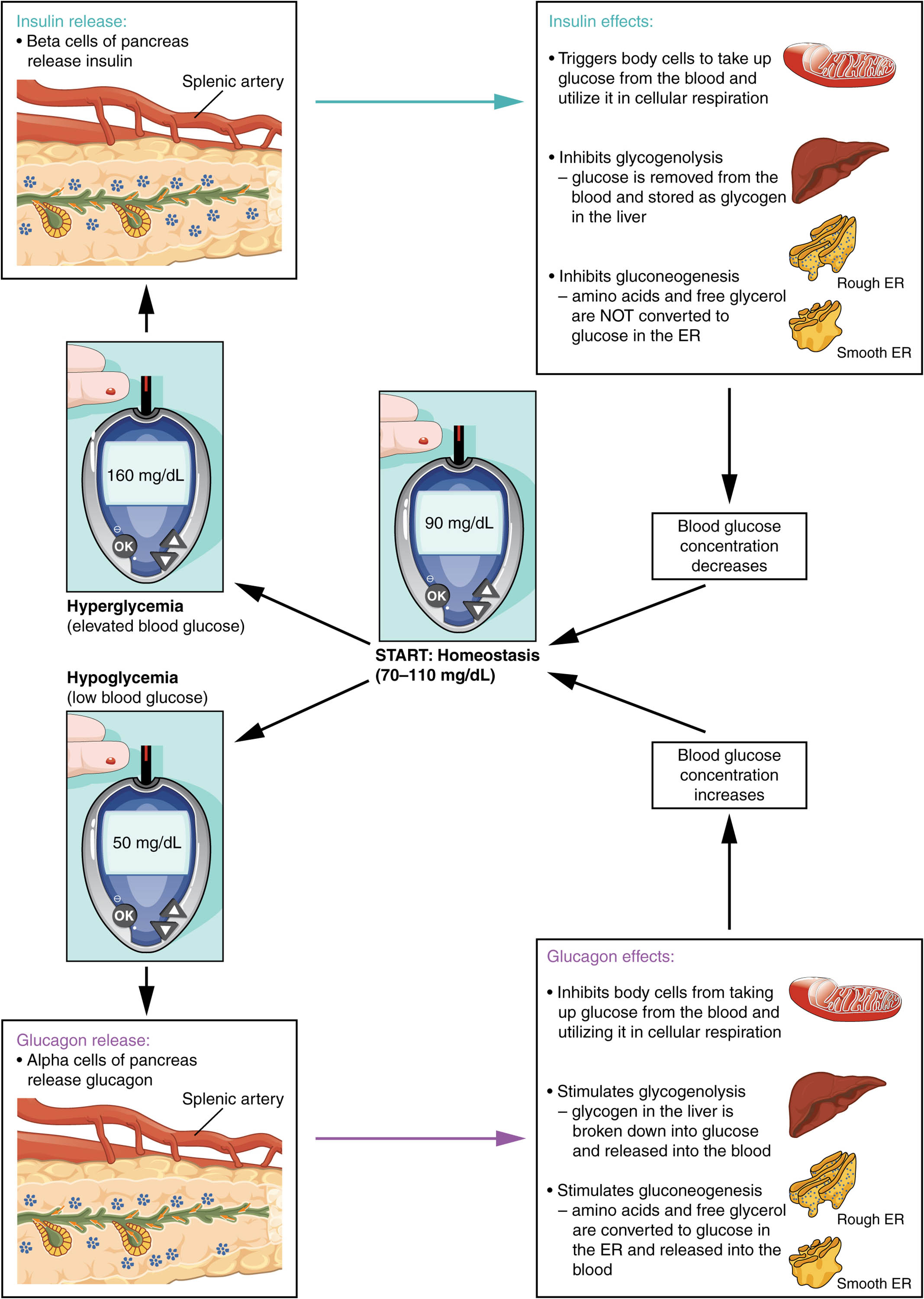
Blood glucose concentration Blood glucose concentration reflects the amount of sugar in the bloodstream, typically maintained between 70 and 110 mg/dL. Fluctuations beyond this range trigger hormonal responses to restore balance.
Normal range (70-110 mg/dL) The normal range of 70-110 mg/dL represents the target for blood glucose homeostasis. This range supports cellular energy needs without causing harm from hypo- or hyperglycemia.
Above normal range (>110 mg/dL) When blood glucose exceeds 110 mg/dL, such as after a meal, it signals the pancreas to release insulin. This condition prompts cells to absorb excess glucose, reducing levels.
Below normal range (<70 mg/dL) When blood glucose drops below 70 mg/dL, such as during fasting, the pancreas releases glucagon. This response stimulates glucose release from storage to raise levels.
Pancreas The pancreas houses endocrine cells that secrete insulin and glucagon to regulate blood glucose. It responds to glucose level changes through its islet cells.
Insulin Insulin, released by beta cells, lowers blood glucose by promoting its uptake into cells and storage as glycogen. It is secreted when glucose levels rise, such as postprandially.
Glucagon Glucagon, released by alpha cells, raises blood glucose by stimulating glycogen breakdown and gluconeogenesis in the liver. It is activated during hypoglycemia to prevent energy deficits.
Body cells Body cells, including muscle and fat cells, absorb glucose in response to insulin. They release glucose into the blood under glucagon’s influence during low glucose states.
Liver The liver stores and releases glucose, playing a central role in glucose homeostasis. It converts glycogen to glucose or synthesizes new glucose based on hormonal signals.
Homeostasis Homeostasis is the process of maintaining blood glucose within the 70-110 mg/dL range through insulin and glucagon. This balance ensures stable energy supply and prevents metabolic disruption.
Overview of Blood Glucose Regulation
The regulation of blood glucose involves a dynamic interplay of hormones. This system ensures energy availability under varying conditions.
- Blood glucose concentration is monitored continuously by the pancreas.
- The normal range supports brain function and physical activity.
- Above normal range triggers insulin release to manage excess sugar.
- Below normal range prompts glucagon to restore glucose levels.
- Homeostasis prevents complications from glucose imbalances.
Role of the Pancreas in Glucose Control
The pancreas serves as the primary regulator of blood glucose through its endocrine cells. Its strategic location enhances its responsiveness.
- The pancreas detects glucose changes via islet cells.
- Insulin from beta cells lowers glucose by enhancing cellular uptake.
- Glucagon from alpha cells raises glucose during fasting.
- This dual hormonal action maintains metabolic stability.
- The organ’s proximity to the liver aids efficient glucose management.
Mechanisms of Insulin and Glucagon Action
Insulin and glucagon target specific organs to adjust glucose levels. Their actions are complementary to maintain balance.
- Insulin stimulates glucose uptake by body cells, reducing blood levels.
- The liver stores excess glucose as glycogen under insulin’s influence.
- Glucagon triggers glycogenolysis and gluconeogenesis in the liver.
- Body cells release stored glucose into the blood when glucagon is active.
- This coordinated response prevents hypo- or hyperglycemia.
Clinical Relevance and Related Disorders
Understanding blood glucose regulation aids in managing metabolic diseases. Disruptions can lead to significant health issues.
- Diabetes mellitus occurs when insulin production or function is impaired, causing hyperglycemia.
- Insufficient glucagon can lead to severe hypoglycemia, risking seizures.
- The pancreas’ role is assessed via glucose tolerance tests.
- Liver function tests evaluate glycogen storage capacity.
- Treatments include insulin therapy or dietary adjustments.
The precise homeostatic regulation of blood glucose between 70 and 110 mg/dL, driven by the pancreas’ release of insulin and glucagon, ensures a steady energy supply for the body. This delicate balance, supported by the liver and body cells, is crucial for health, while conditions like diabetes mellitus highlight the importance of this system. This knowledge provides a foundation for exploring metabolic regulation and effective clinical interventions.

