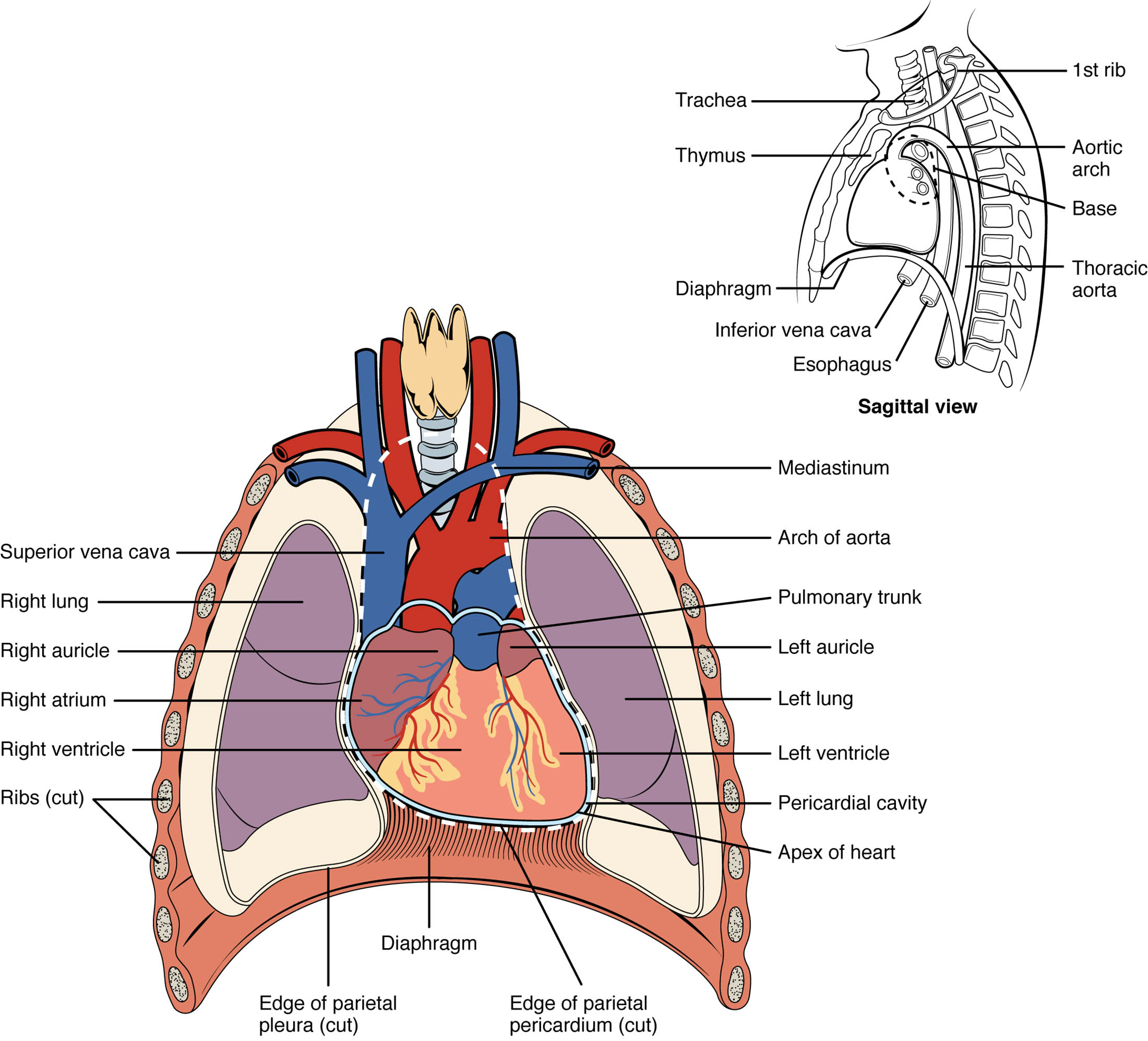
The heart occupies a central role within the thoracic cavity, nestled medially between the lungs in the mediastinum, where it functions as the powerhouse of circulation. This article examines its anatomical placement, roughly the size of a fist, with a broad base at the top and a tapered apex, using a detailed diagram to illustrate its position. Grasping this spatial arrangement enhances understanding of the heart’s relationship with surrounding structures and its critical physiological role.
Thoracic cavity
- The thoracic cavity is the chest region that houses the heart, lungs, and major blood vessels, protected by the rib cage.
- It provides a stable environment, allowing the heart to perform its pumping action efficiently.
Mediastinum
- The mediastinum is the central compartment of the thoracic cavity, containing the heart, great vessels, and other structures.
- It serves as a protective and supportive framework, anchoring the heart between the lungs.
Heart
- The heart is a muscular organ approximately the size of a fist, responsible for pumping blood throughout the body.
- Its position in the mediastinum ensures optimal blood flow to and from the lungs and systemic circulation.
Lungs
- The lungs flank the heart on both sides within the thoracic cavity, facilitating gas exchange.
- Their proximity to the heart supports the pulmonary circulation loop essential for oxygenation.
Base
- The base of the heart is the broad superior portion, located near the second rib, where major vessels like the aorta and pulmonary artery emerge.
- It provides attachment points for the great vessels, anchoring the heart’s upper structure.
Apex
- The apex is the pointed inferior end of the heart, typically resting on the diaphragm near the fifth intercostal space.
- This tapering region marks the heart’s lowest point, influencing its orientation within the thorax.
Pericardium
- The pericardium is a double-layered membrane surrounding the heart, providing protection and reducing friction during heartbeats.
- It anchors the heart within the mediastinum while allowing slight movement with each contraction.
Diaphragm
- The diaphragm is a dome-shaped muscle below the heart, separating the thoracic cavity from the abdominal cavity.
- It supports the heart’s apex and plays a role in respiratory movements that affect cardiac function.
Sternum
- The sternum, or breastbone, lies anterior to the heart, offering a protective barrier within the thoracic cage.
- Its position helps shield the heart from external trauma.
Ribs
- The ribs encase the thoracic cavity, providing a skeletal framework that protects the heart and lungs.
- They allow for chest expansion during breathing, indirectly influencing heart movement.
The heart’s position within the thorax is a key aspect of its anatomical and functional design, enabling efficient circulation and interaction with nearby organs. The diagram highlights its placement in the mediastinum, a central region flanked by the lungs, with the base at the top and the apex pointing downward toward the diaphragm. This orientation supports the heart’s role in pumping oxygenated blood from the lungs and deoxygenated blood to them, maintaining the body’s circulatory balance.
Anatomical Placement: Heart Within the Mediastinum
The heart’s location in the mediastinum is central to its function within the thoracic cavity. This positioning allows for close coordination with the lungs and major vessels.
- The mediastinum houses the heart, great vessels, trachea, and esophagus, creating a compact yet accessible region.
- The heart’s medial placement ensures balanced pressure from the surrounding lungs during respiration.
Structural Features: Base and Apex Orientation
The base and apex define the heart’s unique shape and orientation within the thorax. This structure supports its dynamic role in circulation.
- The base, broad and superior, connects to the great vessels, facilitating blood entry and exit.
- The apex, tapering inferiorly, rests on the diaphragm, stabilizing the heart’s position.
Protective Layers: The Role of the Pericardium
The pericardium encases the heart, offering both protection and mobility within the thoracic cavity. This layer is essential for maintaining cardiac function.
- The outer fibrous pericardium anchors the heart to surrounding structures, preventing excessive movement.
- The inner serous pericardium reduces friction, allowing the heart to beat smoothly.
The heart’s location in the thoracic cavity is a marvel of anatomical precision, positioned medially within the mediastinum between the lungs. The thoracic cavity, enclosed by the ribs and sternum, provides a protective shell, while the diaphragm below supports the heart’s apex. The base, situated near the second rib, is where the great vessels—such as the aorta, pulmonary artery, and vena cava—connect, enabling the heart to distribute blood effectively. The pericardium, a double-layered sac, encases the heart, anchoring it while allowing the freedom to contract and relax with each heartbeat.
The lungs, occupying the lateral spaces of the thoracic cavity, surround the heart, facilitating the pulmonary circulation loop. The mediastinum not only contains the heart but also the trachea, esophagus, and major nerves, creating a complex yet organized compartment. The sternum and ribs form an anterior and lateral protective barrier, safeguarding the heart from external impact. The diaphragm, a muscular partition, supports the apex and moves during respiration, influencing the heart’s position and venous return. This anatomical arrangement ensures the heart operates within a stable yet dynamic environment.
The heart’s size, approximately that of a closed fist, reflects its capacity to handle the body’s blood volume—about 5 liters in an average adult. Its orientation, with the base tilted slightly to the right and the apex to the left, aligns with the body’s asymmetrical design. The pericardium’s fibrous layer attaches to the diaphragm and sternum, while its serous layer secretes pericardial fluid to minimize friction during the cardiac cycle. This fluid, typically 15-50 mL, reduces wear on the heart as it beats around 60-100 times per minute at rest.
The heart’s position also influences clinical assessments, such as auscultation and percussion, where the apex beat is typically heard near the fifth intercostal space, left of the sternum. Imaging techniques like X-rays or echocardiograms often reveal the heart’s silhouette, confirming its mediastinal placement and any deviations due to conditions like cardiomegaly or pneumothorax. The proximity to the lungs allows for efficient gas exchange, as deoxygenated blood is pumped to the pulmonary arteries, while oxygenated blood returns via the pulmonary veins to the left atrium. This close relationship underscores the heart’s dependence on thoracic anatomy.
The mediastinum’s central location provides access for surgical interventions, such as coronary artery bypass grafting, where the heart’s position relative to the sternum and ribs is critical. The diaphragm’s movement during breathing affects intrathoracic pressure, aiding venous return to the heart via the inferior and superior vena cava. The pericardium also plays a protective role against infections or inflammation, such as pericarditis, which can alter its fluid dynamics. Understanding these relationships enhances the ability to interpret physical findings and manage thoracic pathologies effectively.
The position of the heart in the thorax is a testament to its evolutionary design, balancing protection and functionality. Its placement within the mediastinum, supported by the pericardium and surrounded by the lungs, ensures optimal performance in the circulatory system. This anatomical insight not only deepens appreciation for the heart’s role but also informs clinical practices aimed at maintaining cardiovascular health.

