Accurate blood type cross-matching is a cornerstone of safe transfusion medicine, ensuring compatibility between donor and recipient blood. This article examines a commercially produced “bedside” card used for quick ABO+D typing, featuring reaction sites with anti-A, anti-B, and anti-D antibodies to detect blood antigens. Understanding this process is essential for preventing transfusion reactions and optimizing patient outcomes.
SAMPLE
- The SAMPLE label indicates a test sample used on the bedside card for blood typing.
- It serves as a placeholder to demonstrate the testing process with a specific blood sample.
ABO+D
- The ABO+D label signifies the blood typing system, including the ABO group and the Rh (D) factor.
- This combined testing determines the full blood type, such as A+, B-, or AB+, critical for transfusion compatibility.
Anti-A
- The Anti-A well contains antibodies that react with A antigens on red blood cells, causing agglutination if present.
- A positive reaction in this well indicates the blood sample is type A or AB.
Anti-B
- The Anti-B well is coated with antibodies that detect B antigens, leading to agglutination if B antigens are present.
- A positive result here suggests the blood type is B or AB.
Anti-D
- The Anti-D well tests for the Rh (D) antigen, with agglutination indicating Rh-positive status.
- This test is crucial for identifying Rh factors, such as + or -, in the blood type.
Agglutinated RBCs
- Agglutinated RBCs are red blood cells that have clumped together due to an antigen-antibody reaction.
- This visible clumping in a well confirms the presence of specific antigens, aiding in blood type identification.
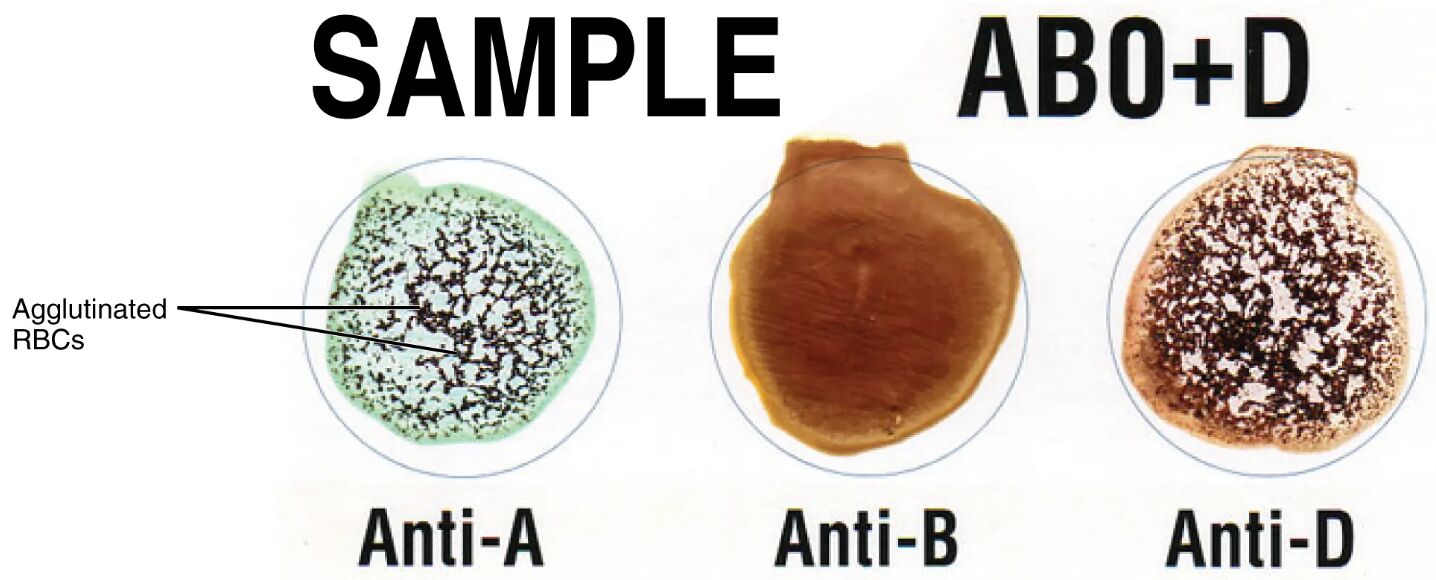
Blood type cross-matching is a vital procedure in transfusion medicine, designed to prevent adverse reactions by ensuring donor and recipient compatibility. The diagram showcases a bedside card with three reaction sites—Anti-A, Anti-B, and Anti-D—where a drop of blood mixed with saline interacts with type-specific antibodies. This rapid testing method allows for quick identification of blood antigens, such as A, B, and Rh (D), which determine the blood type, like A+ in the sample shown. Mastering this technique enhances the ability to manage transfusions effectively and safely.
The Role of Anti-A in Blood Typing
The Anti-A reaction site is a key component of the ABO+D testing process. This well helps identify the presence of A antigens on red blood cells.
- A positive agglutination in the Anti-A well indicates the blood contains A antigens, classifying it as type A or AB.
- No reaction suggests the absence of A antigens, pointing to type B, O, or a variant.
The Role of Anti-B in Blood Typing
The Anti-B reaction site complements Anti-A, targeting B antigens for accurate blood group determination. This step is essential for distinguishing between blood types.
- Agglutination in the Anti-B well confirms the presence of B antigens, indicating type B or AB blood.
- A negative result rules out B antigens, narrowing the type to A, O, or a related group.
The Role of Anti-D in Rh Factor Testing
The Anti-D reaction site assesses the Rh (D) antigen, a critical factor in blood compatibility. This test determines the positive or negative status of the blood.
- A positive reaction in the Anti-D well signifies Rh-positive blood, such as A+ or B+.
- No agglutination indicates Rh-negative status, like A- or O-, influencing transfusion decisions.
The ABO+D blood typing process is a precise method to classify blood based on the presence of A antigens, B antigens, and the Rh (D) antigen, ensuring safe transfusions. The bedside card, a practical tool in clinical settings, features three wells coated with anti-A, anti-B, and anti-D antibodies. When a blood sample is mixed with saline and added to these wells, the antibodies bind to corresponding antigens on red blood cells, causing agglutinated RBCs if a match occurs. This agglutination, visible as clumping, allows for rapid identification of the blood type, such as A+ in the sample, where reactions occur in the Anti-A and Anti-D wells but not Anti-B.
The ABO system, discovered by Karl Landsteiner, categorizes blood into A, B, AB, and O based on carbohydrate antigens on red blood cell surfaces. Type A blood has A antigens and anti-B antibodies, type B has B antigens and anti-A antibodies, type AB has both A and B antigens with no antibodies, and type O has neither antigen but both anti-A and anti-B antibodies. The Rh factor, another critical component, adds a positive (+) or negative (-) designation based on the D antigen’s presence. The Anti-D test on the card detects this antigen, with agglutination indicating Rh-positive status, which is vital for preventing hemolytic disease in pregnancies or transfusions.
The process begins by placing a drop of the recipient’s and donor’s blood into each well, allowing the antibodies to interact with the red blood cells. Agglutination in the Anti-A well confirms A antigens, in the Anti-B well confirms B antigens, and in the Anti-D well confirms the Rh (D) antigen. The absence of agglutination in a well indicates the lack of the corresponding antigen. For instance, the sample shown exhibits agglutination with Anti-A and Anti-D but not Anti-B, identifying it as A+. This pattern ensures the blood type is accurately determined, guiding transfusion compatibility.
Transfusion safety hinges on matching the donor’s and recipient’s ABO and Rh types to avoid immune reactions. An A+ recipient, for example, can receive A+ or O+ blood but not B+ or AB+ due to the presence of anti-B antibodies that would cause agglutination and hemolysis. The bedside card’s speed—providing results in minutes—makes it invaluable in emergencies, such as trauma or surgery, where immediate blood availability is critical. Cross-matching, which involves mixing donor and recipient blood to confirm compatibility, often follows this initial typing to detect additional antibodies or rare antigens.
The Rh factor’s significance extends beyond transfusions to pregnancy, where an Rh-negative mother carrying an Rh-positive fetus can develop anti-D antibodies, leading to erythroblastosis fetalis. Preventive measures, like Rh immunoglobulin (RhoGAM), mitigate this risk by neutralizing fetal red blood cells before sensitization. The ABO+D card’s design, with its clear visual indicators, supports both routine and urgent testing, enhancing clinical decision-making. Regular calibration and quality control of these cards ensure reliable results, minimizing the risk of transfusion errors.
Understanding blood typing also aids in managing transfusion-related complications. Mismatched transfusions can trigger acute hemolytic reactions, releasing free hemoglobin that damages kidneys and activates the complement system. The card’s simplicity allows healthcare professionals to perform testing at the bedside, reducing delays in critical situations. Advanced techniques, like gel card or tube methods, may complement this approach for confirmation, but the ABO+D card remains a first-line tool due to its accessibility.
The ABO+D testing process exemplifies the precision required in transfusion medicine. By identifying agglutinated RBCs and interpreting reaction patterns, one can ensure blood compatibility, safeguarding patient health. This knowledge not only strengthens clinical practice but also highlights the intricate balance of the immune system in blood management.

